Reports
Hyponatremia in Heart Failure: Addressing Sodium and Symptoms
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PRIORITY PRESS - Vascular 2013
Montréal, Québec / October 16-20, 2013
Montreal - Hyponatremia develops in up to 30% patients with heart failure (HF). The condition may be chronic and largely asymptomatic but may worsen during episodes of acute decompensation. The significant negative impact of low serum sodium on prognosis is poorly recognized. In a review of evidence-based recommendations, Canadian HF experts noted that when standard therapies are inadequate, patients with congestion and severe hyponatremia may derive rapid symptomatic benefit from a course of tolvaptan. Monitoring and management of serum sodium should be part of routine follow-up.
Chief Medical Editor: Dr. Léna Coïc, Montréal, Quebec
Hyponatremia is defined as serum sodium <135 mmol/L; sodium <130 mmol/L is considered severe deficiency. In patients with heart failure (HF), hyponatremia results from a relative excess of total body water versus sodium, although both parameters may actually be elevated above normal. Hypervolemic hyponatremia also occurs in patients with cirrhosis and nephrotic syndrome.
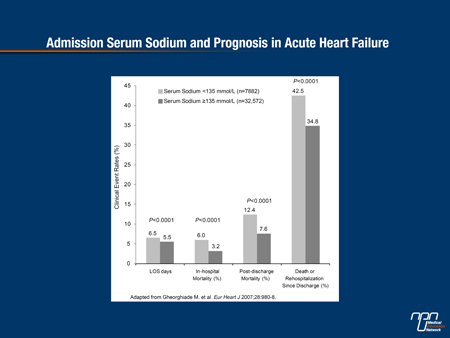
Hyponatremia is more prevalent than is widely perceived among patients with HF and has a negative impact on prognosis, noted Dr. Gordon Moe, Director, Heart Failure Program, St. Michael’s Hospital, Toronto. Data from several studies indicate that between 12% and 30% of patients admitted with acute decompensated HF have a low serum sodium level. The development of hyponatremia during HF hospitalization is also a fairly frequent phenomenon. In both situations, hyponatremia is associated with a longer hospital stay, higher mortality in-hospital and during the 30 days after discharge, and higher rates of a composite outcome of death and rehospitalisation (Figure 1).
The clinical significance of hyponatremia is underappreciated, added Dr. Robert McKelvie, Medical Director, Heart Failure Program, Hamilton Health Sciences, Ontario. “I often see hospital patients hovering around 120 to 127 (mmol/L) and we don’t think much about it. But it’s important to realize that...their potential for survival is significantly reduced and their risk of having other events is higher compared with those who maintain a serum sodium within the normal range.”
Degree Dictates Action
Although milder cases may be asymptomatic, hyponatremia can produce a host of symptoms including nausea, vomiting, headache, fatigue, confusion, irritability, muscle weakness, cramping or spasms, seizures and coma. “As the sodium goes down the prognosis gets worse [and] if it’s symptomatic you should act upon it sooner and more aggressively,” commented Dr. Serge Lepage, Centre hospitalier universitaire de Sherbrooke, Quebec.
In general, according to Dr. Lepage, the target rate of sodium correction should be 8 to 10 mmol within 4 to 8 hours; a shorter time frame of 4 to 6 hours is recommended for severe cases (e.g. patients with central nervous system symptoms). In more chronic or asymptomatic hyponatremia, the aim should be to increase sodium by 12 mmol within 28 hours.
Figure 1
Numerous Strategies
In HF patients with chronic or asymptomatic hyponatremia, treatment options include restrictions on fluid consumption, salt supplementation, or demeclocycline, which blocks the effects of antidiuretic hormone, Dr. Lepage indicated.
The 2012 Canadian Cardiovascular Society guidelines (Can J Cardiol 2013;29:168-81) recommend intravenous (IV) diuretics as first-line therapy for patients with HF and congestion. The diuretic may be administered via intermittent bolus or in a continuous infusion. Interestingly, IV administration of a loop diuretic such as furosemide can be a double-edged sword, noted Dr. Lepage. “Sometimes when you give [IV furosemide] the amount of sodium relative to water will be favourable but sometimes it will get worse.”
If initial therapy for acute HF is insufficient, a number of strategies for fluid volume reduction may be contemplated. Fluid restriction to as little as 500 mL to 1 L a day may be effective, although compliance with this measure can be taxing for patients. Additional pharmacologic agents may include potent diuretics such as metolazone and urea. These also may present challenges: for example, patients’ acceptance of urea is poor due to its unpleasant taste; metolazone can contribute to hyponatremia and hypokalemia. Other measures such as ultrafiltration may be considered. However, in the CARRESS-HF study (N Engl J Med 2012;367:2296-304) ultrafiltration was no more beneficial than medical therapy and led to more adverse events. In fact, ultrafiltration performed without the co-administration of saline led to a statistically significant decrease in sodium as compared with diuresis, cautioned Dr. Jonathan Howlett, Director, Heart Failure Program, Libin Cardiovascular Institute, University of Calgary.
Recent reports suggest that salt supplementation can be effective, although patients with HF are not typically sodium-depleted. Administration of salt tablets both raises sodium levels and encourages fluid loss, Dr. Lepage stated.
Rapid Improvement
The 2012 HF guidelines indicate that tolvaptan should be considered for patients with symptomatic or severe hyponatremia and persistent congestion despite standard therapy to elevate the serum sodium and address related symptoms. Although vasopressin inhibitors such as tolvaptan have not demonstrated the ability to reduce mortality or HF-related hospitalization, clinical trials have demonstrated that a course of this agent (usual dose 15 to 30 mg day) raises and maintains the patient’s sodium level, encourages water weight loss, and improves symptoms such as dyspnea and edema without altering heart rate, blood pressure or renal function (N Engl J Med 2006;355:2099-12; JAMA 2004;291:1963-71). Tolvaptan is very effective in stabilizing serum sodium during intensive HF treatment, stated Dr. McKelvie. “It helps control symptoms, lowers sodium and potentially allows the other therapies to be used in a more effective fashion.”
Tolvaptan is absorbed rapidly and works quickly, said Dr. Howlett. It typically increases sodium by 7 to 8 mmol, as compared with 3 to 4 mmol with fluid restriction alone or with urea. Fatigue and thirst are the principal side effects; fortunately, restrictions on fluid consumption can be relaxed. The patient’s sodium level should be measured after 8 hours, as response to the drug does vary and may influence further dosing. Once sodium has returned to at least 130 mmol/L and the patient’s symptoms have abated, usually within 5 days, the drug can be stopped and the patient monitored, the speakers agreed.
Acknowledging the relatively high cost of tolvaptan, Dr. Howlett added, “it’s really for the most part limited to in-hospital use and the approach I’ve taken is that I reserve it for cases that don’t respond to initial therapy.” In the EVEREST trial (JAMA 2007;297:1332-43), HF patients who received tolvaptan were discharged from hospital about two days earlier than those given placebo. The shorter length of stay may contribute to cost savings, he commented. “This is a drug that will enable you to be more aggressive and it will likely be easier to get the patient to a position where they can go home faster.”
Following Up
A patient who experienced an episode of acute HF should ideally visit a heart failure specialist or clinic shortly after hospital discharge to ensure that appropriate diuresis is continuing. “One reason is when they are in the hospital situation they are well diuresed and invariably they are discharged at a much lower dose of diuretics. If we don’t see them early they will be back in a very short time,” commented Dr. Moe. Education to reinforce self-care practices such as fluid restriction and weight monitoring should be provided to the patient and any caregivers.
Clinicians should keep in mind the possibility and risks of hyponatremia, Dr. McKelvie advised. “Hyponatremia... is one of those ‘sleeping giant’ types of situation. Heart failure patients [tend to] cruise along with lower sodium levels and we don’t do a lot about it. But we should think about the significance and the impact of hyponatremia on patients with heart failure and just rethink our approach to it.”