Reports
Progress and Challenges in Recognizing Inborn Errors of Metabolism Presenting with Neuropsychiatric Symptoms
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
MEDICAL FRONTIERS - Garrod Symposium 2015
Vancouver, BC / May 21-23, 2015
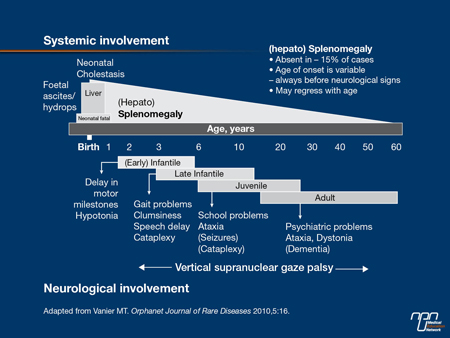
Vancouver - Niemann-Pick Disease Type C (NP-C) often remain undiagnosed or misdiagnosed for > 5 years due to a lack of physician awareness and the rarity and clinical heterogeneity of the disease. Improved awareness amongst psychiatrists and neurologists is crucial for early diagnosis as progressive neurological degeneration and pychiatric symptoms could rapidly arise by the time patients become young adults with this dementing condition. According to Dr. Marc Patterson, who authored the clinical guidelines for NP-C, this is a treatable disease and miglustat therapy, available in Canada, seems most effective when started early. Advances in genetic testing with massively parallel sequencing and the advent of oxysterol biomarkers assay technology are making significant contributions to the screening and diagnosis of NP-C. Most frequent clinical features of NP-C involve systemic, neurological and psychiatric manifestations as well as hepato and/or splenomegaly in newborn and early infantile. The incidence and full spectrum of adult-onset NP-C is not fully understood.
Chief Medical Editor: Dr.Léna Coïc, Montréal, Quebec
Recognizing inborn errors of metabolism (IEM) with neuropsychiatric presentation poses many challenges, said Dr. Clara van Karnebeek, Pediatrician and Biochemical Geneticist at BC Children’s Hospital, at the 2015 Garrod Symposium which she chaired. These challenges include the rarity and unknown frequency of these diseases, their clinical heterogeneity, a lack of awareness amongst physicians and in the case of NP-C access to therapy, explained Dr. van Karnebeek. She emphasized the importance of early diagnosis, using the slogan, “dare 2 care 4 rare!” Niemann-Pick Disease Type C (NP-C) is a treatable IEM and the disease progression can be stabilized if therapy is started early, she maintained. Diagnostic advances include the new biomarkers, oxysterols, which are cost-effective and less invasive than previous methods and allow for early detection of the disease via screening patients at risk. The NPC-Suspicion Index Tool is a useful screening resource as a high score (>70) would indicate the need for further investigation (eg. Filipin test and/or molecular analysis and/or oxysterol assay). “We have a long way to go; it is all about a better understanding of disease mechanisms and translating these into improved care. In 2015, we have emerging omics technologies, digital technologies (www.treatable-id.org) and model organisms at our disposal, which will help advance knowledge in the field,” said Dr. van Karnebeek.
Missed Underlying Genetic Disorders
The World Health Organization estimates that over 10,000 single gene disorders affect 1 in 100 people globally, said Dr. Joyce So, Clinical Geneticist at the University Health Network and Mount Sinai Hospital in Toronto. Amongst neuropsychiatric disorders, for example, up to 40% of autism spectrum patients have an underlying genetic disorder, she said. Dr. So is researching rare disorders in psychiatric populations through genotyping and deep phenotyping to discover “red flags”, markers that could indicate a higher likelihood of rare genetic conditions in psychiatric patients. Educating psychiatrists and other physicians of the important implications of genetic diagnosis will be key and currently presents a big challenge, she said. Awareness of co-existing medical conditions is an important consideration. “Though patients often have other multisystemic findings, their past medical history is often drowned out by details of their psychiatric history,” she said. Many genetic disorders are missed in psychiatric patients, which can lead to a resulting failure of treatment, she explained. When genetic conditions are diagnosed, other affected family members can be screened and treated if need be, she added. Single gene disorders are treatable in many cases and targeting genetic pathways to develop treatment for one disorder can help with others, said Dr. So. Studies show a high diagnostic yield for genetic conditions in “psychiatric plus” patients, explained Dr. So.
Figure 1. Overview of Niemann-Pick C
Massively Parallel Sequencing Used to Diagnose Genetic Disorders with Overlapping Neuropsychiatric Phenotypes
Diagnostic challenges for rare genetic diseases causing neuropsychiatric symptoms include a lack of physician knowledge of these disorders and a belief that they are untreatable, leading to a potential delayed diagnosis or having the condition completely overlooked, said Dr. Sébastien Lévesque, Head, Medical Genetics Laboratories, Centre Hospitalier Universitaire de Sherbrooke. Educating specialists who see neuropsychiatric patients is certainly needed to address this situation, he said. The rate of rare genetic diseases such as Niemann-Pick type C being diagnosed could be further increased if massively parallel sequencing were performed as first-tier clinical diagnostic tool for neuropsychiatric diseases, he explained. Dr. Lévesque described his research with a gene panel of 368 genes for IEMs and other genetic disorders associated with overlapping neuropsychiatric phenotypes (ie; ataxia, dystonia, dementia and psychosis). Bioinformatics analysis revealed a high median coverage of targeted genes within 235-355X (sequences per bases). Single-gene disorders associated with the genes included in the gene panel such as Niemann-Pick type C can be tested specifically for lower price. Compared to exome sequencing, our gene panel covers 100% of targeted exons with high sensitivity and low false positive rates, Dr. Lévesque concluded. For more information on this topic go to [http://www.sherbrookegenomicmedicine.ca]
Oxysterol, new Biomarkers for NP-C
Although the incidence of NP-C is thought to be about 1:100,000, it may be closer to 1:40,000 based on analysis of disease allele frequency in exome databases, said Dr. Daniel Ory, Director, Washington University, St. Louis, who described his work with oxysterols, new biomarkers for the detection of NP-C. NP-C causes cholesterol storage in lysosomes and neuronal cell dysfunction, he explained. With a long diagnostic delay of >5 years, NP-C “has a broader spectrum [of clinical presentations] than we originally recognized,” he said. Patients present with delayed developmental milestones, progressing to psychosis and cognitive impairment as young adults. The discovery of biomarkers began in 2006, using mass spectrometry to phenotype NP-C subjects. Plasma oxysterols were studied initially in mice. Altered plasma oxysterol profiles were later found in human NP-C subjects, i.e. a 9-10 fold elevation compared to control subjects. In a study comparing Filipin assay to oxysterol assay, the oxysterol method was completed in 24 hours versus 2-3 months with the Filipin method. The sensitivity rates were 65% and 97% respectively, and costs were US $2900 for the Filipin assay but only US $100 for the oxysterol testing. The US $100 cost “should be able to be driven down further with larger volumes and running on a regular basis,” said Dr. Ory. The oxysterol test is now offered as CLIA-approved assay through Washington University Metabolomics Facility (http://dcdc.wustl.edu/metab_core.html).The oxysterol assay has been implemented in 12 other institutions globally to date. The Washington University Metabolomics facility is currently working on the technology with the Hospital for Sick Children in Toronto and BC Children’s Hospital in Vancouver, he said.
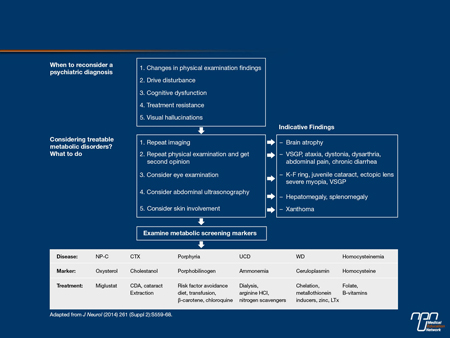
Figure 2. Differential Diagnosis for Patients with Possible Treatable Causes of Organic Psychiatric Disease
Early intervention, why does it matter?
Although only two genes – NPC1 and NPC2 – are associated with NP-C, other genes and pathways may be involved, said Dr. Marc Patterson, Professor of Neurology, Pediatrics and Medical Genetics, Mayo Clinic. Interacting genes, more complex phenotypes and neuronal networks may be important, he said. The NPC1 gene is mutated in 95% of cases and the NPC2 gene, in 5% of cases. The functions of these two genes are not completely understood. Niemann–Pick disease type C
has an autosomal recessive pattern of inheritance, explained Dr. Patterson.
There is an increase in the number of later-onset forms of NP-C presenting with progressive cognitive and psychiatric disorders occurring in teenagers and adults, reported Dr. Patterson. While learning disabilities and expressive language disorders can occur at the onset of NP-C, adolescents and adults present with dysexecutive syndrome. These symptoms sometimes occur “under the radar.” “By the time neurologists make the diagnosis, neurons have been lost and the disease has been present for a long time,” he explained. The whole central nervous system is affected: brain stem, cerebellum, diencephalon, basal ganglia and cortex. Dr. Patterson emphasized the importance of thorough examination in making a clinical diagnosis, and eye movements (vertical supranuclear gaze palsy) are a crucial part of that examination, he said.
“Cognitive symptoms manifesting as developmental delay usually take 6-7 years before diagnosis is made. This process is accompanied by cognitive regression,” reported Dr. Patterson. “NP-C is a dementing illness,” he stressed. Associated psychiatric conditions include mood disorders and schizophrenia-like psychosis. These conditions can be resistant to conventional treatment. However, according to Dr. Patterson NP-C is a treatable disease. “I can’t overemphasize the importance of that,” said Dr. Patterson.
Dr. Patterson discussed the 2014 Bonnot study which highlights key features of 7 treatable inborn errors of metabolism (IEMs) associated with schizophrenia-like symptoms (Diagnostic and treatment implications of psychosis secondary to treatable metabolic disorders in adults: a systematic review. Dr. Olivier Bonnot, Orphanet Journal of Rare Diseases). First level atypical features in schizophrenia suggesting an IEM included confusion, visual hallucinations, catatonia, progressive cognitive degeneration and treatment resistance. Second level symptoms included acute, early onset and intellectual disability. Early MRI findings were usually normal. Abdominal ultrasound detecting hepato-splenomegaly was important in establishing a differential diagnosis. “It is sensitive and available and should be used in a work-up,” he said.
In the ZOOM study, carried out in the EU and US, of 250 patients over 18, 1.2% had NP-C. The study looked at frequency of NP-C in adult patients admitted to neuropsychiatric institutions with a combination of neurological and psychiatric symptoms. Most common neurological symptoms in patients diagnosed with NP-C were dysarthria, ataxia, vertical supranuclear gaze palsy and cataplexy. Two patients diagnosed with NP-C also presented with early onset progressive cognitive decline. Those patients were diagnosed with genetic testing and biochemical analysis.
In a Swiss cohort of 14 NP-C patients from 9 families, who were studied between 1994 and 2013, neuropsychiatric disease patterns were found early, reported Dr. Patterson. These symptoms were present for a long period prior to the diagnosis of NP-C being made. Neuropsychiatric symptoms were universal by the time the patients had reached their late teenage years.
“Why does this matter?” asked Dr. Patterson. Early diagnosis “ends the diagnostic odyssey,” that can consume years, he said. It also makes patients potentially eligible for research studies. Genetic counseling can be offered to parents, allowing them to make informed decisions. “Perhaps in the future we can do carrier screening,” he said.
Regarding management of the disease, Miglustat therapy is most effective when started early, reported Dr. Patterson. Miglustat inhibits glucosylceramide synthase, decreasing sphingolipid accumulation and the drug is usually well tolerated, he said.
Awareness Campaign Targets Physicians
Tammy Vaughn, President, Canadian Chapter of the Niemann-Pick Disease Foundation, described her organization’s “Think Again” awareness campaign, launched in March, 2015. Targeted mailings were sent to neurologists, psychiatrists, paediatricians, neonatologists, paediatric hepatologists and ophthalmologists. The goal of the campaign is to raise the physicians’ awareness of the disease and make earlier diagnoses. A planned second mailing will include a letter from a regional expert in the recipient’s geographical area, along with a Frequently Asked Questions sheet, infographic and an educational slide set. The educational material will describe how to recognize the symptoms of NP-C and what to do if the physician suspects that the disease is present: this approach is also helpful for non-specialist healthcare professionals, said Ms. Vaughn. The website www.think-NPC.ca includes information on where to refer patients, she said.