Reports
Expanding Therapeutic Options in Multiple Sclerosis Treatment: Current Perspectives
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PHYSICIAN PERSPECTIVE - Viewpoint based on presentations from the 5th Joint Triennial Congress of the European and Americas Committees for Treatment and Research in Multiple Sclerosis (ECTRIMS/ACTRIMS 2011)
Amsterdam, The Netherlands / October 19-22, 2011
Guest Editor:
J. Marc Girard, MD, FRCPC
Multiple Sclerosis Clinic
Notre-Dame Hospital
Assistant Professor of Medicine
Université de Montréal
Montréal, Quebec
To see an interview with Dr. Girard, select the "video" icon.
Introduction
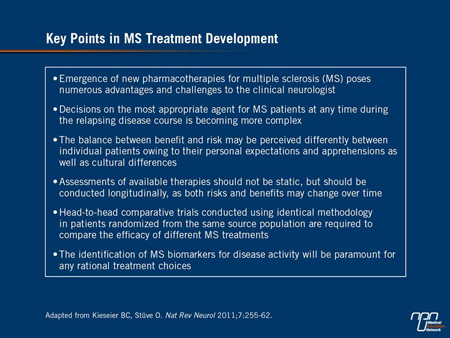
The 2011 ECTRIMS/ACTRIMS congress hosted a large body of new data for an expanding number of therapeutic options in MS, including a growing array of disease-modifying therapies (DMTs) taken orally. New therapies are welcome, but they will require clinicians to weigh the established benefits and risks of the current DMTs with the safety and benefit of new treatments. Newer agents may have immediate application in patients who are not well controlled on current DMTs, such as glatiramer acetate, the interferons and natalizumab, but full integration of the newer agents into evidence-based algorithms will be accomplished gradually. While the encouraging phase III data with newer agents will have better context as longer-term efficacy and safety emerge, it is useful to consider the differences in emerging strategies.
A noticeable amount of phase III data has been recently presented with immunomodulatory agents active in the control of multiple sclerosis (MS). The trial results presented at the 2011 meeting of the American Academy of Neurology (AAN) and the subsequent ECTRIMS/ACTRIMS congress predict a substantial expansion of treatment options over the next few years. Several of these agents can be administered orally. If approved, these will join fingolimod, which recently became the first licensed oral disease-modifying therapy (DMT) in Canada. Acting on a broad array of molecular targets, the expected expansion in DMTs offers a potential opportunity to improve disease control, but it is also important to consider unexpected consequences from altering immunologic pathways. Safety is closely monitored in drug development, but long-term consequences of changes in immune activity may be difficult to predict.
Effects on Immune Function
As an autoimmune process in the central nervous system, MS can be modified by controlling signals of the inflammatory response. The redundant and interrelated inflammatory signals have complicated efforts to understand the precise mechanisms of many therapies. For example, glatiramer acetate (GA) is thought to produce a shift from pro-inflammatory Th1 cells to regulatory Th2 cells that helps suppress the inflammatory response, but other activities are also likely. Similarly, the beta interferons (IFNs) also appear to modulate the profile of cytokine production toward that of the anti-inflammatory phenotype as well as reduce T-cell migration but again, other activities are possible. Regardless of mechanisms, more than 15 years of experience with these established DMTs have generated a large body of efficacy and safety data with which newer agents will be compared.
Like the established DMTs, the precise mechanisms of fingolimod, other emerging oral agents and new injectable agents remain to be fully understood. Even when specific molecular events are known to be affected by these agents, the interrelationship of immune signalling suggests complex alterations in immune function with potential relevance to both efficacy and safety. For the latter, the concern in regard to emerging agents is for unanticipated long-term risks, including potential malignancy, that stem from changes in
immune regulation. The rare but measurable risk of progressive multifocal leukoencephalopathy (PML) from natalizumab and other monoclonal antibodies (MAbs) is perhaps the most notable example of a serious adverse event that was detected only after a substantial clinical experience. In autoimmune diseases, such as psoriasis and rheumatoid arthritis, as well as in cancer, the varied risks of altering immune function are well documented.
Study Evidence
Still, while vigilance for potential risks is needed, the expansion of therapeutic options is expected to improve MS care. New data from the phase III studies with fingolimod continue to provide support for both its safety and efficacy.
One of the most compelling sets of data was provided by pooled results from the phase III FREEDOMS and TRANSFORMS trials performed prior to regulatory approval. At ECTRIMS/ACTRIMS 2011, the pooled data were employed to observe fingolimod efficacy relative to its comparator (placebo in the FREEDOMS trial and IFN beta-1a in the TRANSFORMS trial) in 3 patient groups. These were rapidly evolving severe RRMS patients who were treatment-naive and had had at least 2 relapses in the year before study entry and at least 1 gadolinium (Gd)-enhancing T1 lesion at baseline; or who had been previously treated with IFNs and had at least 1 relapse in the previous year plus at least either 1 Gd-enhancing T1 lesion or 9 T2 lesions at baseline; or who had been previously treated with IFNs and had equal or more relapses in the year immediately before the study than in the 2 years before the study. In all 3 groups, fingolimod provided better control of relapses relative to placebo or IFN beta-1a intramuscular (IM).
During the ECTRIMS/ACTRIMS meeting, phase III placebo-controlled data were presented on teriflunomide, laquinimod and BG-12. Each has a unique purported mechanism of action. All were superior to placebo, and all were relatively well tolerated. However, although these data provide interesting results, they prevent any conclusions to be drawn about relative efficacy either to each other or to existing therapies.
The results with teriflunomide were generated by the phase III TEMSO study, which now has efficacy and safety data extending out to 5 years. This oral agent blocks the enzyme dihydroorotate dehydrogenase, which is important to cell division. The ability to block rapidly dividing cells, including activated T-cells, is a theoretical mechanism for its benefit in MS. In the TEMSO study, which was also recently published (O’Connor et al. N Engl J Med 2011;365:1293-303), 1088 patients were randomized to placebo, teriflunomide 7 mg or 14 mg. The primary end point was annualized relapse rates (ARR), which were 0.54 for placebo and 0.37 for either active dose. In extension data presented at ECTRIMS/ACTRIMS, the relapse rates over a subsequent 3 years of follow-up were 0.182 for those starting on placebo and switching to 14 mg and 0.251 for those started on placebo and switched to 7 mg. The most common side effects during the extension study, similar to the initial 2-year results, were nasopharyngitis, headache and liver enzyme elevations. Serious infections were more frequent but not significantly greater on teriflunomide than placebo.
Recent data on laquinimod from the phase III BRAVO trial were also presented. The mode of action of laquinimod has not been established yet. However, it has been suggested that it may reduce MS severity by turning off pro-inflammatory genes. There is also in vitro evidence suggesting that laquinimod may attenuate MS activity by suppressing genes related to antigen presentation.
In BRAVO, 1331 relapsing-remitting MS (RRMS) patients were randomized to oral laquinimod 0.6 mg q.d. or a matching placebo. Weekly IM IFN beta-1a 30 mcg was offered in a separate, non-blinded reference arm. The primary end point was not reached by laquinimod. The randomization process for BRAVO was adequately performed; however, placebo and treatment study groups showed dissimilarity in two baseline MRI characteristics. According to a standard and pre-specified sensitivity analysis included within the original statistical analysis plan, when this imbalance was corrected, ARR was reduced by 21% (P=0.026) vs. placebo. In addition, laquinimod was associated with a 27.5% reduction in brain volume loss on MRI (P<0.0001) and a 33.5% reduction in the risk of disability as measured on the Expanded Disability Status Scale (EDSS) (P=0.044). In the reference arm of IFN beta-1a, the ARR was reduced 29% (P=0.002) relative to placebo. Laquinimod was well tolerated with no evidence of infections or other immune-mediated adverse events and with a side-effect profile that was not significantly different from placebo.
Phase III data from the DEFINE trial with BG-12 were first reported at the 2011 AAN meeting and updated at ECTRIMS/ACTRIMS 2011. BG-12 is a modified fumaric acid ester. The immunodulatory effects associated with fumaric acid esters have been attributed to their ability to increase glutathione levels. Increased glutathione alters the NF-κB pathway, which is involved in expression of a cascade of inflammatory cytokines and adhesion molecules. In experimental studies, BG-12 has been associated with a variety of changes in cytokine expression by T-cells.
Table 1.
In the DEFINE study, 1237 patients were randomized to BG-12 240 mg b.i.d., 240 mg t.i.d. or placebo. The primary end point was the proportion of patients relapsing at 2 years, which was reduced by 49% by the b.i.d. dose and 50% by the t.i.d. dose relative to placebo (P<0.0001 for both doses). The ARR was reduced by 53% and 48%, respectively (both P<0.0001). Side effects were mild with no increases observed in risk of infections or other immune-mediated adverse events.
Injectable Treatment Strategies
In addition to new oral therapies, there are also new injectable DMTs in development. At ECTRIMS/ACTRIMS, new data were presented on the MAbs alemtuzumab and daclizumab. Alemtuzumab (which already has an indication for the treatment of hematologic malignancies) targets T-cells bearing the CD52 antigen. Although the mechanism of benefit in MS is unclear, experimental studies have associated alemtuzumab with depletion of T- and B-cells in the peripheral blood and lymphoid organs as well as with more modest effects on other immune-activated cell populations, such as NK cells and neutrophils. Daclizumab inhibits the interleukin-2 (IL-2) signalling pathway which is thought to mediate increased activity of T-cells. The clinical significance of these mechanisms of action has not been proven.
In the CARE-MS trial, 581 patients were randomized to alemtuzumab 12 mg/day intravenously (IV), with infusions once a day for 5 consecutive days in year 1 and then infusions for 3 consecutive days for year 2 or to 44 mcg IFN beta-1a administered subcutaneously (SC) 3 times per week for 24 months. The co-primary efficacy end points were relapse rate and time to sustained 6-month accumulation of disability. On the first end point, the MAb reduced relative risk by 55% (P=0.002) compared to IFN beta-1a. On the second end point, there was no significant difference relative to IFN beta-1a. Although discontinuations for side effects were higher on IFN beta-1a (5.9% vs. 1.3%), serious adverse events were more frequent on alemtuzumab (18% vs. 14%). This included a higher rate of serious infections (1.9% vs. 1.1%) and a greater incidence of thyroid problems.
In the SELECT trial, 600 patients were randomized to daclizumab 150 mg SC, 300 mg or placebo administered every 4 weeks. ARR was the primary outcome. At 1 year, these were 0.21 (54% relative reduction vs. placebo; P<0.0001) and 0.23 (50% reduction; P=0.0002) for the lower and higher dose of daclizumab, respectively, vs. 0.46 for placebo (both P<0.001).
Proven Efficacy, Safety of Current Therapies
The substantial activity demonstrated with new agents in these studies is encouraging, but it cannot be presumed that clinical practice will be immediately transformed when or if these agents are approved. One reason is that current therapies offer a proven and established safety and efficacy profile. This conclusion was most recently confirmed by the SAME study, which was presented at ECTRIMS/ACTRIMS. It compared ARR in a Swiss cohort receiving GA or IFN. The rates of ARR were 0.24 for GA, 0.27 for the IM IFN beta-1a, 0.29 for the SC IFN beta-1a and 0.22 for the SC IFN beta-1b. Although this was a retrospective study without a placebo control, the rates are consistent with the large studies that brought these treatments into clinical use. Moreover, they are comparable to the ARR rates reported for the newer agents and less than those typically reported in MS patients randomized to placebo arms.
In the SAME trial, the side-effect profile differed between these agents, but the risk of serious events, including infections, was low, and all of these agents were generally well tolerated. The specific rate of adverse events in the Swiss cohort included flu-like symptoms in 25.7% to 46.7% of those taking an IFN vs. 2.3% for GA. Injection-site reactions occurred in 10.5% of the IM IFN, 26.1% in the GA arm and up to 38.3% in the SC IFN arms.
The introduction of new therapies for MS may eventually alter the treatment algorithms now widely used to prevent disease progression. In general, newer agents will be most attractive for individuals not well controlled on the proven treatments. While the relative risk of serious infections or other short- or long-term complications from newer agents will become clearer with greater clinical experience, the encouraging data with emerging agents suggest a potential for integrating these new therapies into routine MS management strategies to sustain disease control.
Summary
The encouraging results from new DMTs, including new oral agents, are justified but should not overwhelm prudent strategies to achieve an optimal balance of benefit and risk when treating patients. The established benefits of GA and the IFNs in the context of their well-known tolerability and safety profiles should be considered within the effort to understand when to consider newer drugs. While the introduction of new agents for MS is welcome, it is important to proceed rationally with choices guided by needs not fulfilled by current options.
