Reports
Understanding the burden and management of NF1: Insights from SIOP 2023
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PRIORITY PRESS - SIOP 2023: Annual Meeting of the International Society of Paediatric Oncology
Ottawa, Ontario / October 11–14, 2023
Ottawa – The annual conference of the International Society of Paediatric Oncology (Société internationale d’oncologie pédiatrique, SIOP) brought clinicians and researchers from around the world to Ottawa, to share the latest insights into a wide range of paediatric cancers and syndromes. Several posters and presentations focused on the diagnosis, management, and clinical impact of neurofibromatosis type 1 (NF1), a rare autosomal dominant genetic tumour disorder that affects about one in 3000 people. This report will focus on new insights into the burden of NF1 for patients and their families, and the current state of MEK inhibitor treatment for NF1-associated tumours.
“NF1 is a rare genetic disorder, caused by a mutation in the NF1 gene which codes for the neurofibromin tumor suppressor protein,” explained Dr Sébastien Perreault, CHU Sainte-Justine, Montréal.1The key clinical features of NF1 are usually evident in early childhood and are highly variable, but most commonly include skin manifestations (typically café-au-lait macules and abnormal freckling in the skin folds), developmental delays, and a wide range of non-malignant and malignant tumours including cutaneous neurofibromas, plexiform neurofibromas (PN), optic pathway gliomas, and malignant peripheral nerve sheath tumours (MPNST).
Although PN are considered to be benign, they can have a major impact on patients’ symptoms and quality of life. “Depending on the size and location, PN will have a different clinical impact,” said Dr Perreault. “If it's on the face, the patient will have more disfigurement. If it's on the limbs, there's going to be some functional impairment. If it’s in the neck or thorax, it can cause compression of vital structures such as the trachea. Some patients will report significant pain. And about 10% of these lesions will transform into MPNST, which often present with rapid progression and pain.”1
Chief Medical Editor: Dr. Léna Coïc, Montréal, Quebec
Insights into NF1 burden of disease
To better understand the treatment journey and unmet needs of patients with NF and their families, two posters by researchers at Alexion/AstraZeneca Rare Disease used artificial intelligence to detect trends in anonymized data from social media platforms.
The first poster focused on the treatment journey and found that overall, patients and caregivers face significant challenges and delays in getting a definitive diagnosis and being referred to a specialist. In Canada, the symptoms of most concern to patients and families were neurofibromas, followed by neoplasms (Figure 1a). The authors concluded that, “There appears to be a need to enhance diagnosis and, particularly, improve referral to specialists and Centres of Excellence. These findings highlight the need for better communication with patients based on their actual needs (such as pain management).”2
The second poster investigated unmet needs among NF1 patients and families/caregivers. Key barriers to effective diagnosis and treatment included insurance issues; a lack of NF1 specialists; a lack of information, especially for French-speaking Canadians; poor awareness of NF1 among physicians; issues with transitions between paediatric and adult care; and a lack of awareness about treatment options. The most pressing quality-of-life concerns mentioned by Canadian patients and families included disease-related fears, the emotional/psychological burden of disease, and physical pain (Figure 1b). “These findings highlight the need for better communication, and they can help shape awareness campaigns for families and HCPs,” concluded the authors.3
Figure 1: Top NF1-related issues raised by patients, families, and caregivers in Canada
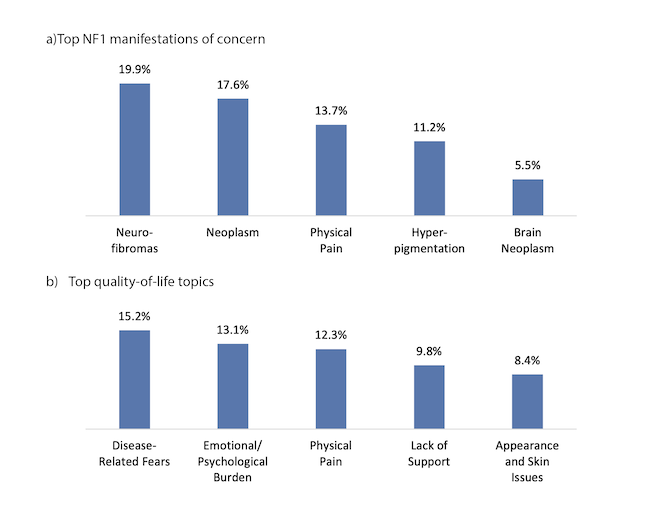
Adapted from: a) Burckhardt S et al., poster A211 at SIOP 20232; b) Efimenko I et al., poster B005 at SIOP 20233.
MEK inhibitors: A new option for PN and a possible future direction for low-grade gliomas
“If we go back about a decade, there was no systemic treatment [for PN] and patients were often referred for surgery,” explained Dr Perreault. “But resection is always a challenge because [PNs are often] wrapped around vessels or nerves, and it's really a small number of patients where we can achieve a total resection. For the rest, there’s an unmet need for a more effective therapy. And this is where the MEK inhibitors really changed the field and the treatment of these patients.”1
MEK inhibitors, such as selumetinib and trametinib, are oral medications that reduce the over-activation of the MAPK/ERK pathway that occurs in NF1. Selumetinib has recently been approved in Canada for treatment of symptomatic, inoperable PN in patients aged 2 and older with NF1; trametinib is currently not approved in NF1.
Dr Andrea Gross of the National Cancer Institute in Maryland reviewed the pivotal phase 1 and 2 clinical data for selumetinib in NF1-PN, along with a recently published long-term follow-up. In the phase 2 study, Dr Gross reported that, “Thirty-four people had confirmed partial responses – at least 20% shrinkage – which was 68% of the cohort. But more excitingly, we were able to demonstrate that after about a year of treatment, 86% of parents and 72% of children reported improvement in their symptoms.”4 In the long-term analysis, about 60% of patients were able to maintain their volumetric response over 12 months of treatment, and the improvement in pain appeared to persist over several years.5 Adverse effects (AEs) were mostly mild to moderate and manageable, with gastrointestinal and skin side effects being the most common.1
MEK inhibitors could also be a valuable treatment option for other tumour types associated with NF1. Dr Perreault presented the results of a phase 2 study of trametinib in patients with recurrence of low-grade glioma (LGG) after initial chemotherapy, which included a cohort (n=12) of patients with NF1. “in general, NF1 gliomas do better than non-NF1 gliomas, so often they can be managed with first-line chemotherapy and they don't need to go for a second line of treatment,” explained Dr Perreault. “But some patients need to restart treatment, and it seems that they respond fairly well to a MEK inhibitor – the response rate depends, but it's over 50%, [encompassing] either minor, partial, or complete response. And we had one really interesting case where [the tumour] completely disappeared.” The AE profile in this study was similar to the previously observed for MEK inhibitors, primarily gastrointestinal and cutaneous effects.6
These results were further supported by a real-world study by Dr David Sumerauer, University Hospital Motol, Prague, and colleagues, who conducted a retrospective review of patients with LGG treated with inhibitors of the MAPK pathway (BRAF inhibitor dabrafenib or MEK inhibitor trametinib). Of the fifteen patients treated with trametinib, 33% achieved a partial response, with a median time to response of 6.6 months. The authors concluded that “MAPK inhibitors represent novel treatment modality in paediatric LGG patients, with clinical benefit in a proportion of patients.”7
Implications and advice for Canadian clinicians
When asked for his key take-aways for Canadian clinicians, Dr Perreault said, “I think the most important aspect is that now we have an efficacious systemic treatment for PN. Surgery is a possibility for some of these patients, but for most it's not. MEK inhibitors really changed the way we manage these patients, and the outcome and natural history. It’s a game-changer for some of these patients, because they have less pain, or they have more mobility, or it changes the cosmetic appearance. And this goes beyond the volumetric analysis - sure, it's nice to see the tumor shrinkage, but it’s even better to see them improve clinically.”
Dr Perreault recommended that HCPs should take the time to have an open and comprehensive discussion with patients and families about the duration of treatment with selumetinib, expected outcomes, and management of side effects. “We have to be transparent and say that we don't know how long treatment will be – it's at least two years, often three. There’s going to be a constant evaluation of response and side effects, and we're going to tailor treatment based on that. Usually, it's well tolerated – there are some significant cutaneous side effects, but they’re manageable. There are different medications – orals or topicals – that can help the patient manage the AEs and get through their whole treatment.“ He mentioned that his clinic builds a strong collaboration with dermatologists to manage skin-related AEs: “When patients come to clinic [with a cutaneous AE], we call the dermatologist and they’re seen right away, and it makes a huge difference for the families.”
Dr Perreault also encouraged collaboration and consultation if HCPs are unsure how to optimally manage patients with NF1. “Every oncology centre has developed their expertise in these lesions, so if a provider is not comfortable with management of PN or gliomas, there's always a nearby paediatric oncology Centre of Excellence that can see the patient and work with the physician to start treatment and guide them throughout treatment,” he said. “It's always possible to reach out and get some advice, but if they're not sure, I think it's always better to refer and then we can start the discussion.”
References
1. Improving care in paediatric patients with NF1-PN: Approaches to disease management in clinical practice. Satellite symposium at SIOP 2023, October 11–14, 2023.
2. Burckhardt S et al., poster A211 at SIOP 2023, October 11–14, 2023.
3. Efimenko I et al., poster B005 at SIOP 2023, October 11–14, 2023.
4. Gross AM, et al., N Engl J Med 2020; 382(15):1430–1442.
5. Gross AM, et al., Neuro Onco 2023; 25(10):1883–1894.
6. Perreault S, et al. Oral presentation at SIOP 2023, October 11–14, 2023.
7. Sumerauer D et al., poster A126 at SIOP 2023, October 11–14, 2023.