Reports
A decade of improved outcomes in aHUS: insights on complement inhibition and special populations
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PRIORITY PRESS - 60th ERA Congress: European Renal Association (ERA)
In-person/virtual, Milan, Italy / June 15–18, 2023
Milan – Atypical hemolytic uremic syndrome (aHUS) is a form of thrombotic microangiopathy (TMA) characterized by microangiopathic anemia with red blood cell fragmentation, thrombocytopenia, and acute kidney injury. Over the longer term, thrombotic damage to the kidney can lead to end-stage renal disease and the need for transplantation. Although aHUS is rare, it is important for clinicians to understand how to distinguish it from other forms of TMA and initiate the appropriate management. At the recent annual congress of the European Renal Association (ERA), more than a dozen poster presentations and a sponsored symposium discussed the latest insights into the diagnosis and management of aHUS; this report will focus on new data about the impact of the C5 inhibitors eculizumab and ravulizumab on aHUS management, and on special considerations for aHUS in pregnancy and pediatric patients.
Chief Medical Editor: Dr. Le´na Coi¨c, Montre´al, Quebec
“All TMAs have a central pathogenic event that consists of severe damage to the vascular endothelium by many different causes,” said Dr Manuel Praga, Hospital Universitario 12 de Octubre, Madrid, Spain, in a sponsored symposium at ERA 2023. He explained that “typical” HUS is generally triggered by infection with certain strains of E. coli. Atypical HUS (aHUS) can be characterized as either:
- Primary or familial aHUS: associated with alterations in genes related to the complement pathway
- Secondary or non-familial aHUS: triggered by external events such as medications, autoimmune causes, viral or pneumococcal infections, malignancy, transplantation, or pregnancy
It is important to distinguish between primary and secondary aHUS, through a thorough clinical workup, complement function testing, genetic testing, and characterization of potential triggers, because understanding the etiology will influence management decisions. “Primary aHUS has a clear relationship with dysregulation of the complement system, so the first-line treatment is C5 blockade with eculizumab or ravulizumab,” said Dr Praga. “In secondary aHUS, the treatment should start with management of the underlying cause – discontinuing a drug, treating autoimmune disease, and so on.” However, he additionally showed that transient complement activation may occur in secondary aHUS, suggesting a possible role for complement inhibitors in conjunction with treatment of the triggering cause.1
Insights into C5 inhibition with eculizumab and ravulizumab
Eculizumab and ravulizumab are inhibitors of the terminal complement component C5 that are the standard of care for aHUS in many countries including Canada. Both are effective at rescuing renal function and restoring hematologic parameters in treatment-nai¨ve and treatment-experienced patients with aHUS. They are administered intravenously: after loading doses every 2 weeks for eculizumab and every 8 weeks for ravulizumab.1
The Global aHUS Registry is an ongoing observational, multinational study collecting real-world data from aHUS patients around the world, including several sites in Canada. An analysis of Registry data by Dr Gema Ariceta, Brigham and Women’s Hospital, Boston, and colleagues showed that over the past 10 years, the delay between aHUS diagnosis and treatment has decreased dramatically, likely due to increased awareness and the availability of C5 inhibitors. The authors noted a drop in the need for dialysis and renal transplant over the last decade, particularly in the pediatric population. They concluded, “Although patients with aHUS are being treated more promptly in recent years than 10 years ago, more work is needed, especially in adults, to move towards optimal clinical practice.”2
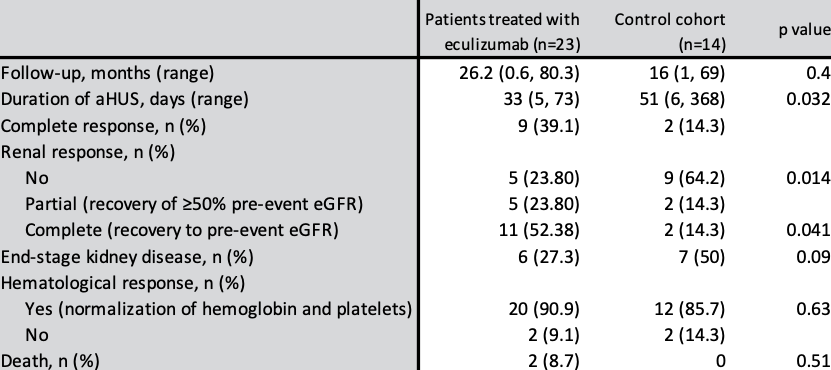
Dr Lucia Cordero, Hospital Universitario 12 de Octubre, Madrid, Spain, presented a poster on her centre’s experience using eculizumab for early treatment of secondary aHUS. The current prevailing practice is to focus on managing the underlying cause of secondary aHUS; in this observational retrospective study, eculizumab was started early regardless of the trigger. After a median of 5 cycles, a significant benefit was observed in the early eculizumab group (n=23) in terms of duration of aHUS and recovery of renal function, compared to the control cohort (n=14) (Table 1). The authors concluded that “Early and short-term use of eculizumab in patients with secondary aHUS could be an effective and safe therapeutic option, ensuring a better renal recovery than treating the underlying cause alone or using other therapies.”3
A presentation by Dr A´lvaro Madrid Aris, Hospital Sant Joan de De´u, Barcelona, Spain, explored the use of ravulizumab for first-line treatment of aHUS in children. “There is still little evidence in the literature of nai¨ve treatment with ravulizumab in pediatrics,” said Dr Madrid, as he introduced two recent cases of successful ravulizumab use in younger patients. The first was a 13-year-old girl who had recently arrived from another country with a one-week history of aHUS symptoms, including acute gastrointestinal symptoms, neurological involvement, and acute renal failure. Upon initiation of ravulizumab, hematologic parameters and renal function recovered rapidly, with a complete hematologic remission within 7 days of the first dose. The second case involved a 7-year-old girl with a lifelong history of aHUS episodes who required kidney transplantation due to stage 5 CKD. She was judged to be at high risk of recurrence of aHUS due to the presence of the MCP gene, inherited from her mother. Her father donated the kidney for transplantation and the patient was given a dose of ravulizumab prior to surgery and a second dose two weeks later. At the time of follow-up, kidney function was stable with no recurrence of aHUS. “The inclusion of ravulizumab in the therapeutic pool opens a new way of safe treatment in pediatric patients with aHUS, demonstrating that it is effective and safe,” concluded Dr Madrid.4
Table 1. Main outcomes according to treatment group in patients with secondary aHUS.
Focus on pregnancy-associated aHUS
Pregnancy-associated aHUS most often presents late in the pregnancy or post-partum, and can have life-threatening consequences. Several posters at ERA 2023 illustrated the importance of prompt diagnosis and management of pregnancy-associated aHUS.
Dr Andrea Spasiano, Universita` Cattolica del Sacro Cuore, Rome, Italy, presented a poster on his centre’s experience with 14 patients who experienced pregnancy-associated aHUS. Possible aHUS triggers included postpartum hemorrhage, intrauterine fetal death, uterine atony, and abruptio placentae. All patients were promptly diagnosed (range of 1-5 days following symptom onset) and treated with eculizumab (mean 27.6 +/- 15.2 hours after diagnosis). All patients gradually achieved recovery of kidney function and normalization of hematologic parameters. Most patients remain on treatment but one has discontinued, with close monitoring. “We hope that these clinical records could help to improve the awareness of this manifold syndrome and to emphasize the importance of an early diagnosis and a timely treatment with eculizumab to guarantee a full recovery,” concluded Dr Spasiano.5
Dr Michael Che, University of Ottawa, Canada, presented two posters, each outlining an instructive case in post-partum aHUS. In the first, a patient who experienced severe HELLP (Hemolysis, Elevated Liver enzymes and Low Platelets) syndrome in late pregnancy showed further decline in renal function post-partum, in spite of the other symptoms resolving. Renal biopsy showed findings consistent with TMA and complement function testing was suggestive of aHUS. “This suggests the patient may be at high risk of developing a recurring TMA, especially if there’s another pregnancy that occurs,” said Dr Che. “Future research is needed to identify which patients with TMA in pregnancy would benefit from complement inhibitors such as eculizumab.”6
The second case involved a patient who presented with hypertension and acute kidney injury unusually early, in the first trimester. aHUS was diagnosed and eculizumab treatment started; further investigation revealed a complement mutation. Post-partum, the patient’s kidney function continued to decline and she eventually needed a transplant; since then, her renal function and hematologic measures have remained normal with continued eculizumab treatment. The authors concluded that, “TMA triggered by pregnancy is not always pre-eclampsia or HELLP syndrome; aHUS should be considered for presentations occurring prior to 20 weeks’ gestation."7
Conclusions
Prompt recognition and characterization of aHUS is crucial for optimal management, in the general population and particularly if it arises during pregnancy. Thanks to increased awareness and the use of the complement inhibitors eculizumab and ravulizumab, outcomes for patients with aHUS are improving but more work is needed to continue these trends. Early treatment may be valuable in both primary and secondary forms of aHUS.
References:
1. What’s new in the management of aHUS? Satellite symposium at ERA 2023, June 16, 2023.
2. Ariceta G, et al. Changes in the clinical characteristics and management of patients with aHUS over 10 years: trends from the Global aHUS Registry. E-poster at ERA 2023, June 14–18, 2023.
3. Cordero L, et al. Rational use of eculizumab in secondary atypical haemolytic uremic syndrome. Focussed oral presentation at ERA 2023, June 14–18, 2023.
4. Madrid Aris A, et al. Ravulizumab "de novo" in pediatric patients with atypical hemolitic uremic syndrome: first worldwide cases. Focussed oral presentation at ERA 2023, June 14–18, 2023.
5. Spasiano A, et al. The multiverse of pregnancy-associated aHUS: triggers, timing and outcomes – a single center experience. Focussed oral presentation at ERA 2023, June 14–18, 2023.
6. Che M, et al. Differentiating postpartum HELLP syndrome from atypical hemolytic uremic syndrome. Focussed oral presentation at ERA 2023, June 14–18, 2023.
7. Che M, et al. Kidney transplantation in early pregnancy-associated atypical hemolytic uremic syndrome. E-poster at ERA 2023, June 14–18, 2023.