Reports
Maintenance Therapy as an Emerging Standard for Improving Survival in Multiple Myeloma
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PHYSICIAN PERSPECTIVE - Viewpoint based on presentations at the 53rd Annual Meeting & Exposition of the American Society of Hematology
San Diego, California / December 10-13, 2011
Reviewed and edited by:
Donna E. Reece, BA, MD, FRCPC
Director, Program for Multiple Myeloma
and Related Diseases
Princess Margaret Hospital
Associate Professor of Medicine
University of Toronto
Toronto, Ontario
Introduction
One of the most important contributors to improving outcomes among multiple myeloma (MM) patients has been the introduction of maintenance therapy. In both younger patients—who undergo a hematopoietic stem-cell transplantation—and older transplant-ineligible patients whose first-line therapy includes one of the novel combination regimens, maintenance therapies have been associated with statistically and clinically significant improvements in hard outcomes, including overall survival in some studies. Importantly, the maintenance strategies reported to date have generally been well tolerated, preserving a reasonable quality of life during the period of longer survival. While the ultimate goal of intensive strategies in younger patients includes potential cure, the success of strategies to prolong suppression of MM in older patients may eventually transform myeloma into a chronic controllable disease.
Treatment strategies for younger and older patients with multiple myeloma (MM) differ markedly but there have been important advances over the last 5 years in both. In patients who are transplant-eligible, which typically means individuals up to 70 years of age in good physical status, the current intensive therapies offer the potential for long-term disease remissions and improvement in overall survival (OS). In older patients, the introduction of 3-drug induction regimens with novel agents has also demonstrated relative OS advantages over previous standards in some trials. In both cases, maintenance therapies offer extended benefits, including the potential for longer OS.
These promising developments have led some experts at the ASH 2011 meeting, including Dr. Antonio Palumbo, Division of Hematology, University of Turin, Italy, to predict that all MM patients, particularly those with a low likelihood of complete remission, would be placed on some form of continuous therapy. This assertion can be based on recently reported improvements in outcome with maintenance zoledronic acid, lenalidomide and bortezomib, all of which have an acceptable tolerability, particularly when administered as single agents in maintenance doses. Combination maintenance therapy may be forthcoming as well. According to Dr. Philip McCarthy, Jr., Director, Blood and Marrow Transplant Program, Roswell Park Cancer Institute, Buffalo, New York, the role of newer agents active against MM may be just as important for expanding options in maintenance as for improving the current standards for induction.
Corroborative Evidence
Updated data from several studies have provided the basis for declaring maintenance a standard for improving MM outcomes. Of those cited by Dr. McCarthy, the MRC Myeloma IX study—which compared zoledronic acid to clodronic acid maintenance after an intensive or non-intensive thalidomide-based chemotherapy regimen—and the IFM 2005-02 study—which compared lenalidomide or placebo maintenance after stem-cell transplantation and lenalidomide consolidation—were considered to be practice-changing. In both cases, the advantage of maintenance therapy was achieved with relatively little toxicity. New data on other maintenance regimens were also presented at ASH 2011.
The data from the MRC Myeloma IX study showing a benefit of zoledronic acid (4 mg IV q4 weeks) over clodronic acid (1600 mg orally daily), when each was combined with intensive chemotherapy in younger patients or non-intensive chemotherapy in older patients, were first published in 2010 (Morgan et al. Lancet 2010;376:1989-99). Newer data were presented at the 2011 European Multidisciplinary Cancer Congress showing a benefit from maintenance therapy even after disease progression. In the originally reported findings, patients randomized to zoledronic acid had their median survival extended by 5.5 months (P=0.01184) relative to those randomized to clodronic acid. In the newer data evaluating relative differences in patients who remained on treatment after disease progression, the intravenous agent was associated with a median relative OS advantage of 7 months (34 vs. 27 months; P=0.03) (Figure 1). The OS advantage remained significant even after adjusting for the effects of skeletal-related events (SREs) (HR 0.85; 95% CI, 0.74-0.97; P=0.018). The 2-month relative progression-free survival (PFS) advantage (HR 0.88; 95% CI, 0.80-0.98; P=0.0179) in the initial report was sustained in extended follow-up. The advantage of zoledronic acid was consistent across gender and International Staging System (ISS) class.
Figure 1.
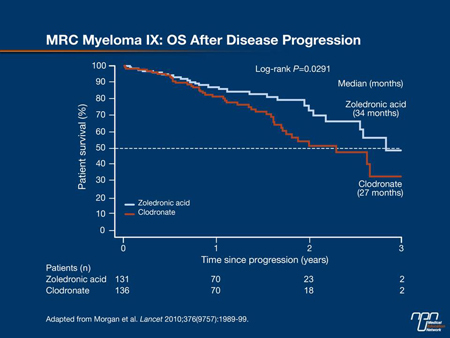
Subgroup Analyses
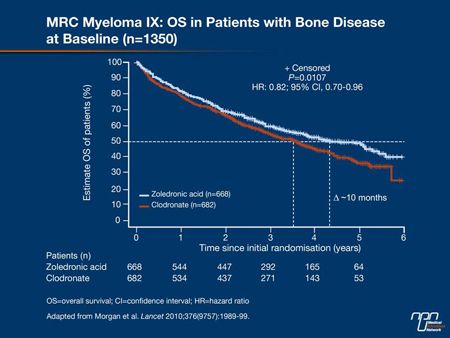
The subgroup analyses of the MRC Myeloma IX study have demonstrated that the survival advantages were concentrated in the patients with bone disease at randomization (who represented approximately 70% of the study population). In these, the 17% relative survival advantage (HR 0.83; P=0.01) translated into about a 10-month extension in survival that persisted through the 6 years of follow-up (Figure 2). In the subgroup without bone disease, no survival advantage was observed.
However, the protection against SREs—defined as vertebral fractures, fractures at other sites, spinal cord compression—was significantly augmented and the requirement for radiation or surgery to control bone lesions was significantly reduced regardless of baseline bone disease status. This included patients with bone lesions at baseline (34.9% vs. 42.8%; P=0.0031) and those without bone lesions (9.6% vs. 17.4%; P=0.0069). Reductions in new bone lesions among those with lesions at baseline (5.7% vs. 11.4%; P=0.00002) and those without (2.3% vs. 5.8%; P=0.035) were also significant. Moreover, when calculated starting at 2 years of treatment, the relative protection from SREs remained significant (P=0.0102) for the subsequent 42 months of follow-up.
Figure 2.
The evidence for a substantial clinical benefit of zoledronic acid over clodronic acid irrespective of bone lesions at baseline is rendered even more clinically meaningful by the low rate of adverse events on this treatment. Both agents were well tolerated in the MRC Myeloma IX study. The only significant difference between these 2 agents in the rate of serious adverse events (SAEs) was related to the induction chemotherapy. In those receiving non-intensive chemotherapy with cyclophosphamide, thalidomide and dexamethasone
(C-TD), 58% of the zoledronic acid patients vs. 45% of the clodronic acid patients (P<0.05) had an SAE. A higher rate of osteonecrosis of the jaw (5% vs. 1%; P<0.05) appears to explain some of this difference; however, the results of newer studies with lenalidomide and bortezomib, typically combined with melphalan and prednisone, suggest that the C-TD regimen may become an uncommon combination for transplant-ineligible patients in the future.
Significant PFS Advantage
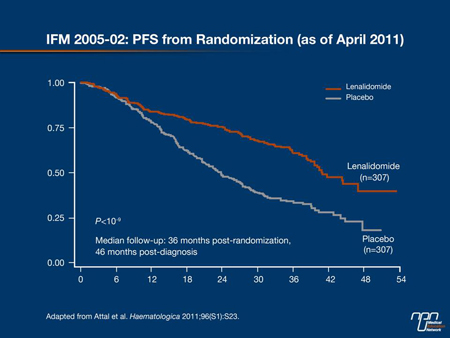
In the phase III multicentre IFM 2005-02 study, 614 patients who had non-progressive disease after an autologous stem-cell transplant were randomized after 2 cycles of lenalidomide consolidation (25 mg/day for 21 days of 2 28-day cycles) to 10 to 15 mg of daily lenalidomide or placebo maintained until relapse. The primary end point of the study was PFS. The results, presented at the 2011 International Myeloma Workshop (IMW) by Dr. Michel Attal, Hôpital Purpan, Toulouse, France, were highly significant. After a median follow-up of 36 months, the OS was not significantly different, but the PFS was improved by more than 25% (P<0.000000001) (Figure 3).
Figure 3.
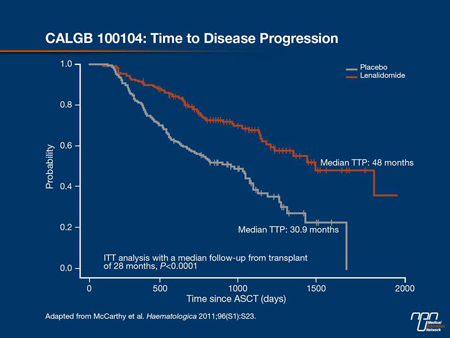
Similar results were generated by the CALGB 100104 study presented at the same meeting by Dr. McCarthy. In that study, patients were also randomized to placebo or lenalidomide 10 mg daily after autologous stem-cell transplant. The primary end point in this study was time to progression (TTP). With a median follow-up of 28 months after transplant, there was almost a 50% improvement in TTP with the active maintenance agent (48 months vs. 30.9 months; P<0.0001) (Figure 4). In this case, OS also reached statistical significance (P=0.018), and there was also a significant advantage for event-free survival (EFS) (43.4 vs. 30.9 months; P<0.0001). Lenalidomide in both of these studies was well tolerated, although quality-of-life analyses are pending.
In transplant-ineligible patients, maintenance therapy with immunomodulating agents like thalidomide and lenalidomide are also delivering promising improvements in outcome. One of the first studies to demonstrate the advantage compared PFS in newly diagnosed patients who received an induction regimen of bortezomib, melphalan, prednisone and thalidomide (VMPT) followed by bortezomib and thalidomide (VT) maintenance or VMPT induction alone. Initially presented by Dr. Palumbo at the 2009 ASH, the PFS advantage at 3 years was 42% (P=0.007). In the second phase III data with a less complicated regimen—presented at the 2011 ASH meeting also by Dr. Palumbo—patients were randomized to 1 of 3 groups. Two of them received an induction regimen of lenalidomide, melphalan and prednisone (RMP) and 1 received melphalan plus prednisone (MP). One of the RMP induction regimens was followed by lenalidomide maintenance (RMP-R), while the other 2 were followed by placebo.
Again, the PFS advantage of maintenance was substantial. After an average follow-up of 30 months, the median PFS was 31 months for RMP-R vs. 14 months for RMP and 13 months for MP, producing a 60% relative advantage (HR 0.395; P<0.001). Importantly, the 3-drug regimen followed by maintenance was well tolerated. The discontinuation rate for adverse events was higher in the arm receiving RMP than MP (13% vs. 4%), but the most common side effects were hematologic and had a minimal effect on quality of life. In fact, although grade 4 neutropenia developed during induction in 39% of patients receiving RMP vs. 7% of patients taking MP, febrile neutropenia did not occur in more than 1% of any treatment arm.
Figure 4.
In a separate study presented at the 2011 ASH with a different design and a variation on the agents used for induction and maintenance, the preliminary results were very similar. The data on maintenance, presented by Dr. Maria-Victoria Mateos, Hospital Clínico Universitario, Salamanca, Spain, represent the second part of a randomization that initially compared different strategies for induction. In the induction phase, which has already been published, the combination of VMP was found equivalent to VTP (Mateos et al. Lancet Oncology 2010;11:934-41). In the maintenance phase, both arms received bortezomib (1.3 mg/m2 on days 1, 4, 8 and 11 in an q3-month cycle) in combination with either 50 mg daily of thalidomide (VT) or 50 mg of every-other-day prednisone (VP).
In the preliminary results, the most important finding was that both maintenance therapies increased the depth of the response observed after the induction regimens, raising the complete response rate from 24% at the end of induction to 42% at the most recent follow-up. Although the response rates, including the complete response rates, were consistently higher on VT vs. VP, the differences in PFS or OS did not reach statistical significance (P=0.1 for both) except in those with high-risk cytogenetics. In this subgroup there was a significant advantage for VT. The ongoing study will provide a more detailed comparison of the relative advantages and disadvantages of VT and VP for maintenance when the median follow-up is complete.
The observation that both VT and VP can deepen the quality of response after induction therapy is a key finding that will likely drive the next generation of studies attempting to identify the optimal sequence of induction and maintenance treatments. For example, while bisphosphonates are typically administered to reduce skeletal events in MM, the experimental evidence that zoledronic acid has anticancer effects was supported by the MRC Myeloma IX study which associated it with an improvement in survival. Strategies that combine bisphosphonates with novel agents such as lenalidomide or other newer immunomodulators or bortezomib and other newer proteasome inhibitors have the potential to further extend disease control with reasonable risk of adverse events.
There is speculation, articulated by Dr. Paul Richardson, Dana-Farber Cancer Institute, Boston, Massachusetts, that future combinations will be rationally designed to address the evolution in disease, particularly in older, transplant-ineligible patients for whom eventual relapse is inevitable. With the most effective front-line combinations, objective response rates are now near 100%. When followed by maintenance regimens to render the responses to first-line therapy deeper and more durable, current data suggest that the time to first relapse can be prolonged. At relapse, second-line therapies may be driven by such considerations as the aggressiveness of the disease or cytogenetics, but rational combinations may be derived from both the response and the toxicities observed with the first-line therapy. As the array of novel therapies with different mechanisms of action increase, it may eventually be possible to select therapies to target specific molecular mechanisms. In all cases, an acceptable tolerability remains critical to extended survival with a preserved quality of life.
Summary
The improved efficacy of first-line induction therapies for both transplant-eligible and -ineligible MM patients was an important first step to the extended control now conferred by maintenance therapies. The recent data that correlated administration of the bisphosphonate zoledronic acid with longer PFS and OS compared with clodronic acid also demonstrated better outcomes with continued therapy even once disease progression occurred. The advantage for survival was achieved with both low toxicity as well as protection against SREs. In updated data of VT or VP maintenance, both combinations were able to increase the objective response rates achieved at the end of induction therapy. These data suggest a new paradigm in MM therapy in which combination or single agents are employed sequentially—before disease progression—to inhibit growth of the MM cell line whithout damaging hematopoiesis or the bone marrow microenvironment. While the optimal sequence of therapies may evolve as the number of agents expands and the molecular targets are better understood, continuous therapy for sustained disease control, with an acceptable quality of life, now represent a useful component of MM management.