Reports
More Aggressive Strategies for Early Detection of Pulmonary Hypertension Supported by Outcome Trials
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
MEDICAL FRONTIERS - 36th Annual Congress of the European Society of Cardiology (ESC)
Barcelona, Spain / August 30-September 3, 2014
Barcelona - Pulmonary arterial hypertension (PAH) should be treated earlier and more aggressively, according to a new analysis of clinical trials with mortality and morbidity endpoints. By demonstrating that outcomes are better when treatment is initiated at an early stage of disease, these studies have produced a reorientation that includes early diagnosis through screening of at-risk populations. It moves PAH management from a palliative approach... to an active early therapy with the intention to halt or slow disease progression. In addition to placing an emphasis on early detection, the revised approach to PAH is encouraging earlier introduction of combination therapies that address multiple pathways of vascular resistance. The controlled trials are consistent with the premise that it is possible and beneficial to treat beyond functional improvements such as the 6-minute walk distance.
Chief Medical Editor: Dr.Léna Coïc, Montréal, Quebec
A large body of evidence, including a new meta-analysis, suggests that effective pulmonary arterial hypertension (PAH) therapies prevent clinical worsening. The evidence further suggests that relative protection is greater when treatment is initiated earlier rather than later in the course of disease progression. This has generated a reorientation in PAH management broadly supported by recently published updated recommendations from the 5th World Symposium on Pulmonary Hypertension. At the 2014 ESC, emphasis was placed on diagnosing PAH at early stages in order to maximize the benefit of current treatment options.
“There is now substantial evidence supporting the value of early treatment in PAH to improve long-term prognosis,” maintained Dr. Nazzareno Galiè, Head, Pulmonary Hypertension Centre, Institute of Cardiology, University of Bologna, Italy. As first author of the management recommendations generated by the 5th World Symposium (Galiè et al. J Am Coll Cardiol 2013;62:D60-72), Dr. Galiè reported that the shift in the paradigm for the detection and management of PAH was made possible by trials that have employed morbidity and mortality endpoints.
The most influential of these trials was completed last year (Pulido et al. N Engl J Med 2013;369:809-18). This trial, called SERAPHIN, was the first multicenter, long-term study to employ morbidity and mortality as the primary endpoint. Functional class (FC) II or III PAH patients were randomized to one of two doses of the novel dual endothelin receptor antagonist (ERA) macitentan or placebo. The majority of patients were on a background therapy (a phosphodiesterase 5 [PDE5] inhibitor in 61.4%; oral or inhaled prostanoid in 5.4%), but a substantial minority (36.3%) was treatment-naïve.
45% Morbidity and Mortality Reduction
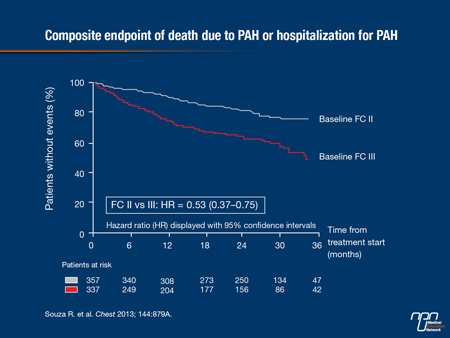
The 10 mg dose of macitentan reduced mortality and morbidity by 45% (P<0.001) relative to placebo over a mean study duration of approximately 2 years, but the benefit was greatest in those who were initiated on therapy at an early stage. Specifically, the risk of death or hospitalization due to PAH was 47% lower in those in FC II at baseline than those in FC III (see figure 1).
Figure 1. SERAPHIN: Patients in FC II at Baseline have a Better Prognosis Compared with Patients in FC III
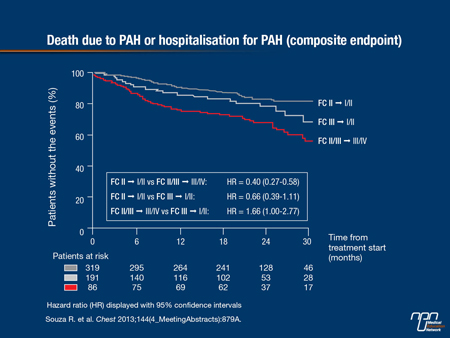
Moreover, improvement in FC on therapy in SERAPHIN was associated with better outcomes so that those in FC II at baseline who remained in FC II or improved to C I had a 60% relative reduction in risk of having a clinical event relative to those in FC II or III at baseline who progressed to FC III or IV (see figure 2).
Figure 2. SERAPHIN: Improvement in FC is Positively Associated with Better Outcomes
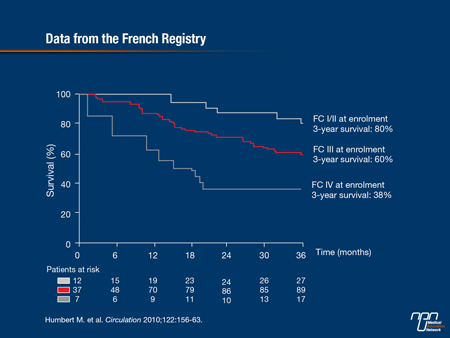
The findings were anticipated by previously published data, such as those from a French registry, which associated each higher FC class at the time of enrolment with a stepwise reduction in survival at three years (Humbert et al. Circulation 2010;122:156-63). Specifically, survival at 3 years fell from 80% in those in FC I or II to 38% in those in FC IV (see Figure 3). Similar data were generated from a registry in the UK (Condiffe et al. Am J Respir Crit Care Med 2009;179:151-7).
On the basis of this and other evidence, “It should now be considered imperative to diagnose PAH early in its course,” reported Dr. Stephan Rosenkranz, Senior Physician, Heart Center, University Hospital, Cologne, Germany. According to Dr. Rosenkranz, this includes screening at-risk populations, such as those with connective tissue disorders, congenital heart disease, or chronic liver disease. While he cautioned that not all target populations are at sufficient risk of PAH to make screening cost-effective, new screening strategies, such as the DETECT algorithm (Coghlan et al. Ann Rheum Dis 2014;73:1340-9) can narrow the proportion of patients referred for definitive diagnosis with right heart catheterization.
Figure 3. FC is Associated with Survival
New Algorithm for Early PAH Detection
“The DETECT algorithm is based on risk assigned from six non-echocardiographic variables, which determines the need for echocardiographic referral. Risk scores assigned from echocardiography are then employed to consider catheterization,” Dr. Rosenkranz explained. Citing the recent study assessing this algorithm, he reported that only 4% of PAH diagnoses were missed with DETECT versus 29% when the ESC/ERS criteria were applied. He and Dr. Galiè anticipate greater application of screening strategies on the basis of the value of early therapy.
For initial therapy in FC II, six therapies were included in recommendations developed at the 5th World Symposium. These were the ERA agents macitentan, ambrisentan, and bosentan, the PDE5 inhibitors sildenafil and tadalafil, and the soluble guanylate cyclase (sGC) inhibitor riociguat. For FC III, intravenous epoprostenol was also included. Although Dr. Rosenkranz emphasized that there are no large multicenter studies providing data on relative benefit of available therapies, he noted that macitentan and epoprostenol were the only ones to be assigned to the list on the basis of a mortality and morbidity benefit, providing an evidence basis for selecting these therapies to reach treatment goals. Previously, treatments for PAH were approved on the basis of short-term effect on 6-minute walk distance (6MWD).
“Baseline 6MWD values are prognostic, but there is now substantial evidence that change in 6MWD from baseline on treatment does not correlate with long-term outcomes and is not a useful endpoint for evaluating treatment efficacy,” Dr. Galiè reported.
Early Intervention May Halt Disease
While functional improvements reflected by a favourable change in 6MWD may have been a reasonable goal in advanced PAH, the attention to therapies that improve long-term outcomes has been intensified by efforts to initiate treatment at an earlier stage of disease, when there may be a greater opportunity to halt or reverse the disease processes. It is likely that the majority of trials evaluating therapies for PAH in the future will evaluate benefit on clinically meaningful events over an extended period.
The opportunity for better outcomes with early treatment were strongly reinforced by the SERAPHIN data. In fact, outcomes tended to be better when macitentan was employed as a single agent in early disease than in patients with advancing disease, according to Dr. Galiè. Specifically, the composite endpoint of hospitalization or death due to PAH was reduced 77% (P<0.001) in newly diagnosed patients, termed the incident group, versus 62% (P=0.026) in patients diagnosed more than 6 months earlier who had not yet started PAH therapy, termed the prevalent group. The reductions in the primary composite endpoint were 55% and 38%, respectively.
“The evidence that the treatment effect is greater in newly diagnosed patients underscores the importance of initiating therapy as early as possible,” Dr. Galiè reported.
Evidence-Based First-Line Therapies
Commenting on choice of initial therapy, Dr. Olivier Sitbon, Professor of Respiratory Medicine, Hospital Antoine Béclère, University of Paris South, France reported that there are several variables that may suggest selecting one therapy over another, but he also identified macitentan as an evidence-based choice on the basis of the SERAPHIN trial. In particular, he concluded that macitentan would be his choice “when an endothelin receptor antagonist is indicated.”
Early initiation of treatment appears to offer the best potential for long-term control of PAH, but there is a general consensus that treatment regimens should be intensified rapidly by adding a second class of PAH therapy if disease is progressing. This has been an important change made in the most recently released treatment guidelines and is consistent with the goal of slowing disease progression, not just relieving symptoms.
“The recommendation for sequential combination therapy to meet treatment goals was given a level 1A recommendation at the 5th World Symposium, which I think highlights a paradigm shift in PAH management,” reported Dr. Irene Lang, Professor of Vascular Biology, Medical University of Vienna, Austria. After initiating therapy with a single agent, she recommends re-evaluating patients at three months to determine whether there have been adverse changes in prognostic indicators, such as hemodynamics, cardiopulmonary exercise testing, or right ventricle morphology on echocardiography. She, like others, emphasized the evidence that a delay in control produces worse outcomes.
Meta-Analysis Supports Combination Therapy
Combination therapy was also supported by a newly completed meta-analysis presented at the 2014 ESC (Abstract 68), which evaluated 10 trials published since 2006. Presented by Dr. Alessandra Manes of the University of Bologna, a 14% reduction in mortality from combination therapy relative to a background single agent did not reach statistical significance (P=0.47), but the 51% reduction (P<0.001) in clinical worsening did.
“The results of this meta-analysis suggest a consistent and statistically significant reduction in the incidence of clinical worsening in patients treated with a combination regimen relative to those treated with monotherapy,” Dr. Manes reported.
The best combination therapy has not been established. Although it is logical to assume greater control of PAH by combining two agents with different mechanisms of action, few studies have compared combinations directly. Rather, most of the evidence supporting combination therapy is derived from trials that evaluated the effects of adding a new agent to an existing background regimen. These have included ERA agents with PDE5 inhibitors and oral prostanoids with ERA agents. Again, only a proportion of these studies were conducted using a morbidity and mortality endpoint. The only combination considered contraindicated is riociguat with a PDE5 inhibitor.
Only One Combination Contraindicated
“A study we initiated with riociguat and sildenafil had to be terminated before it was completed due to an unacceptable rate of adverse events,” reported Dr. Galiè. In the registration trial with riociguat, which tested the effect of this therapy on 6MWD at 12 weeks (Ghofrani et al. N Engl J Med 2013;369:330-40), background therapy with an ERA or prostanoid but not a PDE5 inhibitor was permitted.
The optimal time to initiate combination therapy also remains poorly understood. Several experts at the 2014 ESC referred to goals of treatment. These may be limited to functional improvements in advanced disease, but there is an increasing effort to identify reliable indicators of disease stabilization, such as preservation of cardiac index or other hemodynamic measures. Standardized strategies are needed to identify patients with advancing disease who require more aggressive regimens, including moving from a two-drug to a three-drug combination.
“One important point is that the tolerability of most combinations has been quite good in the clinical trials,” Dr. Lang reported. Although she would not now initiate a combination therapy in patients who appear to be doing well on a single agent, she is closely following ongoing trials that are evaluating first-line combination therapies even in early stage disease. The accumulating support for early combination therapy is accompanied by a rational assumption that combining agents with different mechanisms of action will control disease progression.
Conclusion
Trial data demonstrating that active therapies can reduce the long-term morbidity and mortality of PAH has shifted best care strategies. According to data summarized by multiple experts speaking at the 2014 ESC, earlier intervention in PAH improves long-term outcome. This places new emphasis on the need for early detection of PAH, including screening in high-risk populations. Initial treatment choices now include agents that have been proven to slow clinical worsening, not just provided functional improvements, in long-term randomized treatment trials. This has encouraged goal-oriented therapy. While a single agent may be sufficient to control symptoms and slow progression when initiated in FC II patients, there is increasing emphasis on moving quickly to combination regimens when progressive disease is not controlled on a single agent.