Reports
New Frontiers in IBS Gut Pain Treatments
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
EMERGING INNOVATIONS - November 2023
Regulora® – Digital Therapeutic for Irritable Bowel Syndrome
Irritable Bowel Syndrome in Canada
Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder, characterized by recurrent abdominal pain or discomfort in combination with disturbed bowel habits in the absence of identifiable organic cause. It is considered a functional disorder where complex neuroimmune and brain-gut interactions occur. IBS affects about 10% of the world’s population and shows a similar prevalence in Canada.1 IBS typically is diagnosed by the Rome IV set of diagnostic criteria, which includes abdominal pain associated with defecation (≥1 day per week for ≥3 months) associated with change in bowel habit for at least three months and can be further subtyped by stool consistency. Treatment strategies existing for IBS are largely focused on symptom amelioration and although beneficial, are rarely curative.
Figure 1: IBS Classifications
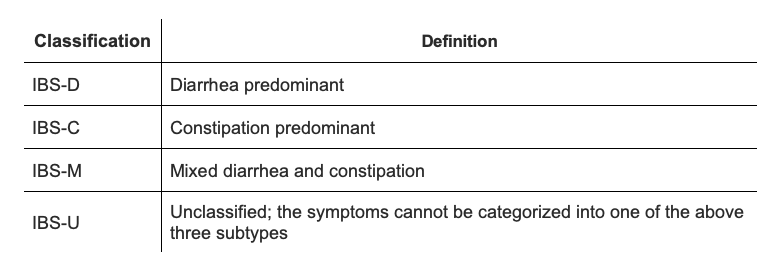
Lacy B E, Mearin F., and L. Chang. "Bowel Disorders Gastroenterology 2016;(150): 1393-1407."
Multimodal Treatment of IBS
Treatment of IBS includes diet modification, pharmaceutical, and psychological therapies, although consensus is low on the effectiveness of any one strategy alone. Patients may benefit most from taking an individualized, multipronged approach incorporating multiple strategies. Interestingly, two of the most recommended pharmacologic treatment options for IBS include low-dose tricyclic antidepressants and selective serotonin reuptake inhibitors, highlighting the major role the gut-brain axis plays in IBS pathology.1 While pharmaceutical strategies exist, it is important to note that clinical responses are reported in less than 70% of patients with approved therapies, indicating that combination therapeutic approaches may be required.2 A variety of strategies exist for psychological therapy in IBS, including cognitive behavioral therapy, relaxation therapy, multi-component psychological therapy, hypnotherapy, and dynamic psychotherapy. A systematic review evaluated 11 different therapy approaches, and overall, psychological therapy was statistically significantly superior to placebo.3 The Canadian Association of Gastroenterology Clinical Practice Guideline suggests using psychological strategies, such as gut-directed hypnotherapy, as an effective treatment for IBS, as outlined in the for the Management of Irritable Bowel Syndrome (IBS): "Cognitive behavioral therapy and hypnotherapy are suggested psychological therapies…"1 However, access to individuals who are trained in psychological therapeutics is extremely limited, especially in Canada, where we have a shortage of healthcare professionals.
What is Regulora®?
Regulora® is a gut-directed hypnotherapy based on the North Carolina Protocol which is the leading psychological strategy studied for IBS. Regulora® is the only app authorized by the FDA and Health Canada for the treatment of IBS. The North Carolina Protocol was developed by Dr. Olafur Palsson, has been tested in multiple published research studies, including the in the EASITx clinical trial, and found to benefit more than 80% of patients.4, 5 In an article currently in press in the journal Clinical Gastroenterology and Hepatology, “A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome”, authors report the results of a 378-patient prospective randomized controlled clinical trial of Regulora® vs a digital muscle relaxing protocol.6 After 12 weeks of treatment, ~30% of patients’ abdominal pain responded to Regulora® treatment, and a greater proportion of patients’ pain reduction reported using Regulora® compared to the digital muscle relaxation protocol (29.3% vs 18.8%; P = .0254). Patients across all IBS subtypes studied (C,D,M, and U) reported improvement in abdominal pain, stool consistency, and stool frequency. The findings support a role for Regulora® in the integrated management of IBS.
According to Dr. Dhandapani Ashok, pediatric gastroenterologist and medical advisor, “gut-directed hypnotherapy (GDH) is a highly effective brain-gut behavioral therapy which is recommended in international guidelines for the treatment of IBS. Clinicians caring for IBS patients increasingly recognize the value of GDH as part of integrated care alongside medical and dietary approaches. A smartphone-delivered app like Regulora® is an innovative, safe, and cost-effective treatment option that provides self-directed GDH skills to modulate pain and psychological responses of the IBS patient.”
Figure 2: Proportion of abdominal pain responders during post-treatment weeks 13-16 (primary endpoint) (A) and treatment weeks 9-12 and 1-13 (entire treatment period) (B)
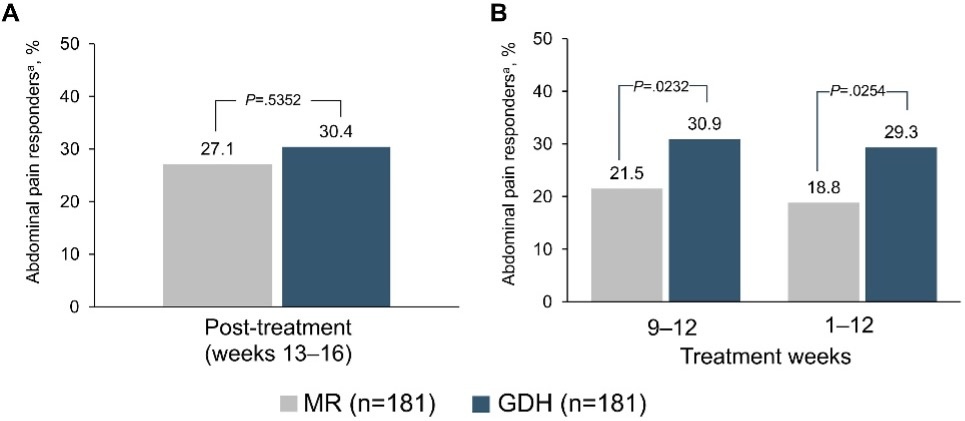
Berry et al. “A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome” Clinical Gastroenterology and Hepatology https://www.cghjournal.org/article/S1542-3565(23)00500-1/
Note
If you are interested in self-guided gut-directed hypnotherapy, Regulora® is available to help treat abdominal pain associated with IBS. It is a digital therapeutic, i.e., a mobile app, that offers one 30-minute session every other week for a total of 7 sessions, along with access to other resources.
Regulora® is now available in Canada for a one-time fee of $200, which may be reimbursable under some health benefit plans. For any Canadian doctors interested in experiencing the Regulora® app, we are offering a complimentary access code that allows them full use of the Regulora® app.
You can refer a patient to Regulora® through their online platform: https://referrals.regulora.ca/.
More information for healthcare providers can be found at https://hcp.regulora.ca.
References
1. Moayyedi et al. “Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS)” Journal of the Canadian Association of Gastroenterology (2019) https://academic.oup.com/jcag/article/2/1/6/5290372
2. Ponti, Fabrizio “Drug Development for the Irritable Bowel Syndrome: Current Challenges and Future Perspectives” Front Pharmacol (2013) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3561631/
3. Ford et al. “Effect of Antidepressants and Psychological Therapies in Irritable Bowel Syndrome: An Updated Systematic Review and Meta-Analysis” The American Journal of Gastroenterology (2019) https://journals.lww.com/ajg/fulltext/2019/01000/Effect_of_Antidepressants_and_Psychological.11.aspx
4. Palsson, Olafur “Standardized hypnosis treatment for irritable bowel syndrome: the North Carolina protocol” Int J Clin Exp Hypn (2006) https://pubmed.ncbi.nlm.nih.gov/16316883/
5. Efficacy and Safety of IBS Digital Behavioral Treatment (EASITx) NCT04133519 https://clinicaltrials.gov/ct2/show/results/NCT04133519
6. Berry et al. “A Randomized Parallel-group Study of Digital Gut-directed Hypnotherapy vs Muscle Relaxation for Irritable Bowel Syndrome” Clinical Gastroenterology and Hepatology https://www.cghjournal.org/article/S1542-3565(23)00500-1/
7. Lacy BE, Pimentel M, Brenner DM, Chey WD, Keefer LA, Long MD, Moshiree B. ACG Clinical Guideline: Management of Irritable Bowel Syndrome. Am J Gastroenterol. 2021 Jan 1;116(1):17-44. doi: 10.14309/ajg.0000000000001036. PMID: 33315591.