Reports
Hyponatremia: Optimizing Clinical Approaches
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
PRIORITY PRESS - 15th International Congress of Endocrinology and 14th European Congress of Endocrinology (ICE-ECE)
Florence, Italy / May 5-9, 2012
Florence - A series of recent studies, including those presented here at the ICE-ECE, are providing evidence-based strategies for the treatment of hyponatremia. Presentations at this year’s congress suggest that a comprehensive and systematic diagnostic workup is essential to enable accurate evidence-based therapeutic management according to the severity of symptoms, duration of the condition and therapeutic objectives. The key is to treat the underlying cause of hyponatremia, which is frequently underdiagnosed and a preventable source of morbidity and mortality. According to recent studies, control of the antidiuretic effects of vasopressin on the renal tubule often has a beneficial role in the context of early diagnosis and supportive care.
Chief Medical Editor: Dr. Léna Coïc, Montréal, Quebec
The key to successful treatment of hyponatremia, which is the most common electrolyte disorder, is to adopt an individualized approach based on accurate clinical diagnosis and follow an evidence-based therapeutic intervention. Here at the ICE-ECE congress, Dr. Chris Thompson, Professor of Endocrinology, Beaumont Hospital, Dublin, Ireland, observed that the lack of evidence demonstrating that restoration of normonatremia improves outcomes has been one barrier to more aggressive management of hyponatremia. However, new data are helping to outline effective treatment algorithms with agents directed at the underlying mechanism of the electrolyte disturbance.
Hyponatremia: Challenges
Hyponatremia, defined as a serum sodium (Na+) concentration <136 mmol/L, occurs in 15% to 30% of all acutely and chronically hospitalized patients (Am J Med 2007;120(11A):S1-S21). Nevertheless, it is frequently diagnosed and managed incorrectly, often as a result of a failure to order sufficient diagnostic tests (Postgrad Med J 2006;82:216-9). In the absence of prompt and accurate management, acute severe hyponatremia can cause substantial morbidity and mortality, especially among those with underlying disease (Am J Med 2007). Research suggests that even asymptomatic hyponatremia is associated with neurocognitive disturbances, gait instability, falls and increased risk of osteoporosis, resulting in bone fractures in the elderly (Am J Med 2006;119:71.e1-8, Q J Med 2008;101:583-8, Clin J Am Soc Nephrol 2010;5:275-80, J Bone Miner Res 2010;25(3):554-663, Biol Chem 2011;286(12):10864-75). The economic burden is twofold: in addition to increased duration of hospital stay (Clin Endo 2006;64:250-4, PMJ 2009;85:171-5, Clin Endo 2006;65:246-9), hyponatremia increases direct medical costs at 6 months (41.2%) and 12 months (45.7%) (J Am Soc Nephrol 2008;19:764-70).
Treatment Algorithm for Euvolemic Hyponatremia
In the treatment algorithm for euvolemic hyponatremia proposed by Dr. Thompson, hypertonic NaCl administration, followed by fluid restriction or a vaptan (vasopressin V2 receptor antagonist) is indicated for this severe symptomatic condition involving vomiting, seizures, obtundation, respiratory distress and coma. Moderate symptoms, including nausea, confusion, disorientation and altered mental status, may be managed with a vaptan or hypertonic NaCl administration, followed by fluid restriction. Asymptomatic or minimally symptomatic hyponatremia involving headache, irritability, inability to concentrate, altered mood and depression can be treated with fluid restriction, but a vaptan should be considered under select circumstances. However, as Dr. Thompson stressed, “Care must be exercised in using tolvaptan following another treatment for hyponatremia and co-administration of tolvaptan with other medicines designed to increase serum sodium is not recommended.”
Explaining the rationale behind his algorithm, Dr. Thompson pointed to the “complete resolution of symptoms with resolution of hyponatremia” in a series of published trials. This includes a study of 223 patients with thiazide-induced hyponatremia whose symptoms correlated with the degree of hyponatremia (J Natl Med Assoc 2004;96:1305-8). In this study, symptoms resolved when hyponatremia was controlled. In another, improvement in SF-12 Mental Component Score was associated with effective treatment of hyponatremia (N Engl J Med 2006;355:2099-112). In a third, treatment of hyponatremia produced an improvement in gait (Am J Med 2006;119:71.e1-8 ).
In the post-hoc analysis of SALT1 and SALT2 (Study of Ascending Levels of Tolvaptan in Hyponatremia), patients treated with tolvaptan showed an earlier discharge, with a 3.7-day reduction in length of hospital stay compared with placebo (Eur J Endocrinol 2011;164:725-32). On the other hand, patients not specifically treated for hyponatremia had higher mortality than those who were (37% vs. 13%) (Nephrol Dial Transplant 2006;21:70-6).
Comprehensive Diagnosis:
Key to Optimizing Treatment Strategy
As delegates heard during the congress, in order to optimize patient treatment and achieve the best possible outcome, a correct etiologic diagnosis is the essential first step. Given that hyponatremia may have several etiologies, especially in elderly patients with comorbidities and/or multiple drug treatments, a comprehensive diagnosis should include clinical history, present condition and drug prescription(s). The diagnostic algorithm must include a baseline assessment of serum toxicity, urine osmolality, volume status and urinary Na+ levels before instituting any medical intervention (Am J Med 2010;123:652-7) (Figure 1).
Figure 1.
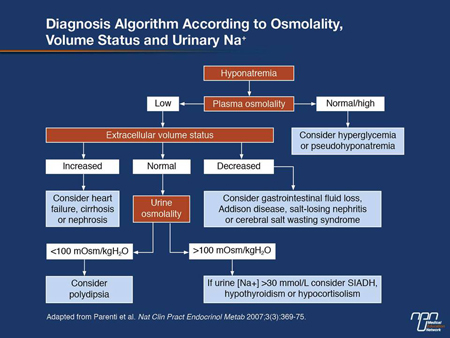
In addition to renal, adrenal cortex and thyroid function assessment, “a key issue in the underlying etiology of hyponatremia is represented by the estimation of the patient’s volume status, which is best assessed by the measurement of central venous pressure,” according to Prof. Alessandro Perri, Professor of Endocrinology, Department of Clinical Physiopathology, Centre for Research, Transfer and High Education on Chronic, Inflammatory, Degenerative and Neoplastic Disorders for the Development of Novel Therapies (DENOThe), University of Florence, Italy. Since this is an invasive procedure and not always available, a thorough physical examination is essential, as is a biochemical analysis for blood urea and creatinine in an effort to distinguish hypovolemic from euvolemic hyponatremia, he explained. Such a diagnostic strategy is essential for appropriate therapeutic intervention (Am J Med 2007;120:S1-S21).
Common Errors in the Routine Management of Hyponatremia
In an interactive bi-directional exercise to characterize current approaches to diagnosis and treatment of hyponatremia in real-life clinical scenarios, the barriers to more effective treatment were highlighted with appropriate case studies. According to these cases, common errors include failure to use hypertonic saline with symptoms of severe hyponatremic encephalopathy; failure to correctly differentiate between hypovolemic and euvolemic hyponatremia; persistent attempts to fluid-restrict, or salt load, despite inadequate response to these therapies; infusion of isotonic saline in the absence of decreased urine [Na+] levels or clinical hypovolemia; and a generalized failure to monitor serum [Na+] frequently during active correction of chronic hyponatremia.
Treating Hyponatremia Secondary to SIADH
Hyponatremia secondary to the syndrome of inappropriate secretion of antidiuretic hormone is one of the most common causes of hyponatremia. Treatment strategies should be guided by the severity of the hyponatremia, according to Dr. Joseph G. Verbalis, Professor of Medicine and Physiology and Chief of Endocrinology and Metabolism, Georgetown University, Washington, DC. For severe symptoms, hypertonic saline is the only treatment that should be employed. Prior to vaptans, fluid restriction was used for mild and asymptomatic conditions and hypertonic saline for moderate symptoms. For mild and moderate symptoms, tolvaptan is appropriate and is the only treatment that targets the arginine vasopressin receptor.
Dr. Verbalis cautioned that correction of hyponatremia with active therapies should be limited to <10-12 mmol/L in 24 hours and to <18 mmol/L in 48 hours, with serum [Na+] monitored at least every 6 hours during the initial days of therapy. He added that patients should be monitored for response to therapy (symptom level, improvement in serum sodium concentration) and assessed for need for continued therapy or a change in therapy.
Summary
A comprehensive diagnostic evaluation is essential to facilitate the initiation of the most appropriate treatment of hyponatremia. With several ongoing studies investigating the treatment of hyponatremia, the evidence base for management of hyponatremia is increasing significantly.

Mednet reports which have been accredited by McGill University under the MedPoint Accredited Conference Report Series are eligible for Mainpro-M1 and MOC Program credits.
© 2012 Mednet Inc. All rights reserved. Priority Press™ is an independent medical news reporting service providing educational updates reflecting peer opinion from accredited scientific medical meetings worldwide and/or published peer-reviewed medical literature. Distribution of this educational publication is made possible through the support of industry under written agreement that ensures independence. Views expressed are those of the participants and do not necessarily reflect those of the publisher, McGill University or the sponsor. No claims or endorsements are made for any products, uses or doses. Specific medicines or treatment strategies discussed in this publication may not yet be approved in Canada. Prior to prescribing any medication, the complete prescribing information in Canada, including indications, contraindications, warnings, precautions, and adverse effects should be consulted. No part of this publication may be reproduced in any form or distributed without written consent of the publisher. Information provided herein is not intended to serve as the sole basis for individual care. Our objective is to facilitate physicians’ and allied health care providers’ understanding of current trends in medicine. Your comments are encouraged.
| Mednet Inc. | 132 chemin de l’Anse, Vaudreuil, Quebec J7V 8P3 | www.mednet.ca |