Reports
New Frontiers in the Control of Influenza
This report is based on medical evidence presented at sanctioned medical congress, from peer reviewed literature or opinion provided by a qualified healthcare practitioner. The consumption of the information contained within this report is intended for qualified Canadian healthcare practitioners only.
MEDICAL FRONTIERS - Canadian Immunization Conference 2023
“Mind the Gap": Getting back on track with influenza vaccination following the global COVID-19 emergency
Ottawa – In normal times, the Canadian Immunization Conference (CIC) takes place every two years, bringing together public health officials, community advocates, and researchers and clinicians with an interest in vaccines and vaccine- preventable diseases. Due to the COVID-19 pandemic, the conference had not taken place in person since 2018 – in part due to restrictions on travel and gatherings, but also because many attendees were heavily involved in managing the most wide-ranging public health crisis of our time, including the largest mass vaccination campaign in human history. CIC 2023 was a long-awaited opportunity to appreciate the efforts and successes of the response to COVID-19, and to look ahead to how advances in vaccine technologies and improvements in public health processes might help us close a significant gap in immunizations against other vaccine-preventable diseases that occurred over those years. This report will focus on presentations and perspectives relevant to routine immunization programs against seasonal influenza in Canada.
Chief Medical Editor: Dr. Léna Coïc, Montréal, Quebec
Lessons Learned from the COVID-19 Pandemic
“As with many crises in history, important lessons and innovations emerged during the pandemic,” said Dr. Theresa Tam, Chief Public Health Officer of Canada and one of the leaders of Canada’s COVID-19 response, in her opening address. “The global vaccine achievements were numerous, including developing new vaccines with new technologies in record time, improving our understanding of vaccinology, more effective delivery of vaccines, and enhanced monitoring of vaccine safety and effectiveness.”
One of the key themes of the conference was the fact that the COVID-19 pandemic, and the associated public health restrictions and stresses on the healthcare system, have created a situation where we need to regain lost ground on vaccination targets for influenza and other vaccine-preventable diseases. The target rate for seasonal influenza vaccination is 80% for adults over 65 and younger adults with chronic conditions, but several speakers highlighted recent survey data from the Public Health Agency of Canada that revealed that these targets were not being met pre-pandemic (70% for seniors and 44% for higher- risk younger adults), and that the rate fell even lower during the pandemic for younger individuals with comorbidities, to a low of 38%.
Dr. Tam also described how the public awareness about vaccines and disease increased during COVID-19, and encouraged her colleagues to consider this new reality when implementing vaccination programs. “I think we mustn't underestimate the capacity of individuals to learn, and their level of interest,” she said. “We should be careful not to simplify things too much – now the public wants communications in a very transparent way about [vaccine] effectiveness, and especially about safety.”
Priority Populations and Goals for Vaccination
Although most provinces and territories in Canada have a policy of universal influenza vaccination across all age groups, there is a particular focus on protecting older adults and those with comorbid conditions that raise the risk of serious outcomes following influenza infection. “Older adults are not simply adults who have been alive for a longer period of time. They are a special group,” said Dr. Melissa Andrews, Dalhousie University, Halifax. She described the phenomenon of immunosenescence, whereby the body’s capacity to mount an immune response declines with age, and also emphasized the impact of comorbidities and a person’s overall level of frailty on their capacity to recover from a bout of infectious disease. “We often think of infections like influenza, or even COVID, as a short-term thing – you get it, you get over it, and then you get better,” she said. “But vulnerable, frail people might not get back to baseline, and could be at risk for persistent functional decline.”
An analysis by Philip Kim and colleagues at Sinai Health in Toronto evaluated the risks and outcomes of influenza in adults between ages 50 and 64. “The incidence of severe illness due to influenza doesn’t change dramatically at the [65-year] breakpoint,” said Mr. Kim. This prospective, population-based surveillance study for laboratory-confirmed influenza (LCI) and illness outcomes found that individuals aged 50-64 were hospitalized for LCI at an annual rate of 22.4 per 100,000 (versus 7.49 for younger adults and 45.9 for those 65+), and had annual mortality of 0.90 per 100,000 (versus 0.12 for younger adults and 2.0 for those 65+). In particular, underlying illness was associated with an elevated risk of hospitalization or death due to LCI, in 50-to-64-year-olds as well as those 65+. (Figure 1)
Figure 1. Hospitalization and mortality rates in 50-64 and 65-74-year-olds with and without underlying illness
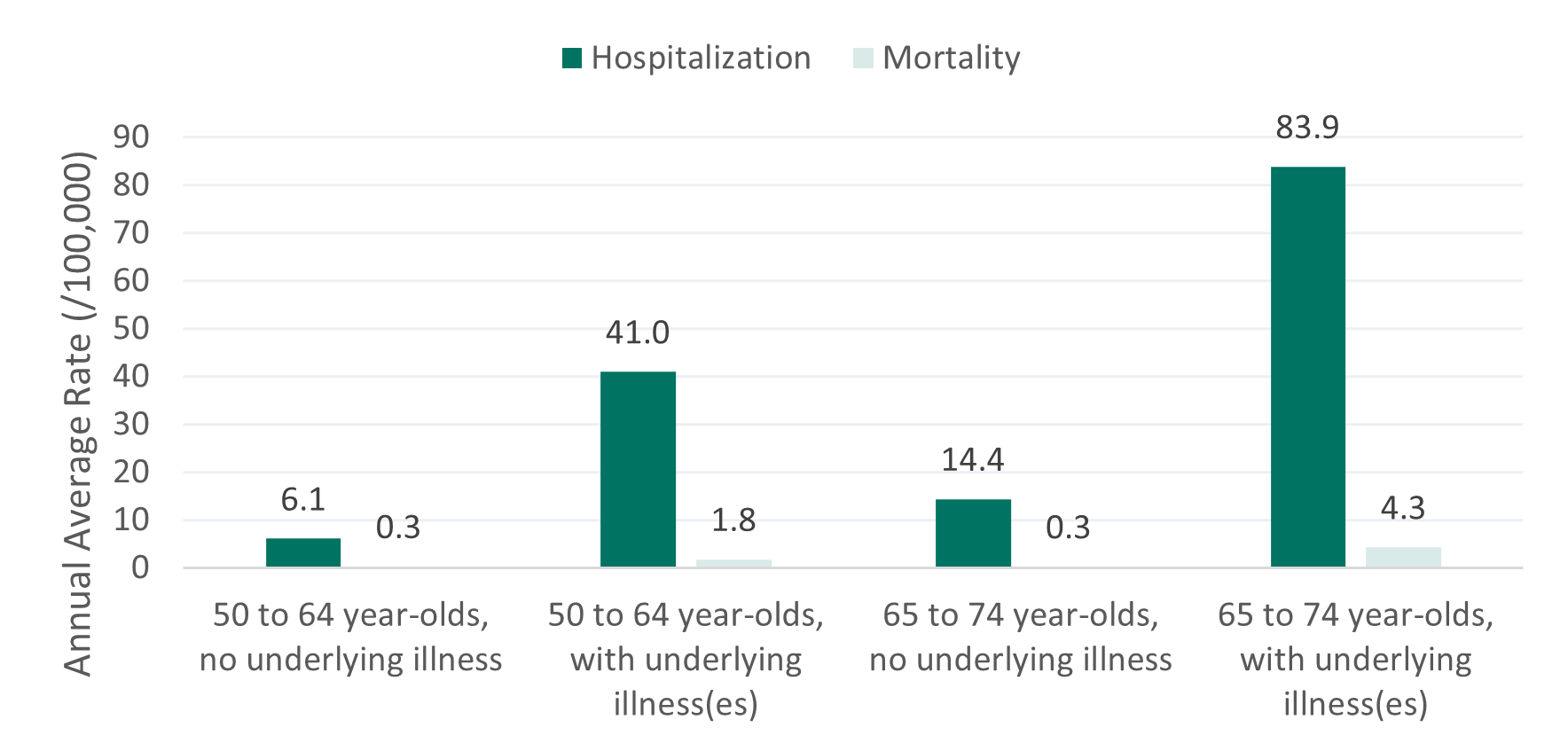
Reference: Adapted from Kim D et al., oral presentation at CIC 2023.
Although the central goal of influenza vaccination is to prevent respiratory-related severe outcomes and death, emerging evidence suggests that the benefits could extend beyond respiratory outcomes into the cardiovascular system. In a sponsored symposium, Dr. Philippe De Wals of Université Laval in Québec described how severe respiratory infections can increase cardiovascular risk by promoting a pro-inflammatory and pro-coagulant state. The risk of myocardial infarction transiently increases by about 6-fold in the week following LCI in adults, and in global estimates, influenza activity has been estimated to contribute to approximately 4% of all mortality attributed to ischemic heart disease. Dr. De Wals reviewed data showing a protective effect for influenza immunization against myocardial infarction and cardiovascular death, particularly in people with existing cardiac risk factors. “This emerging concept that influenza vaccination could protect against cardiovascular diseases may change the way we promote these vaccines and talk about their cost-effectiveness,” he concluded.
Currently Available Vaccines
“Influenza immunization used to be simple – we just said, ‘get the flu vaccine’ – but now there are a lot more options,” said Dr. Scott Halperin of the Canadian Centre for Vaccinology at Dalhousie University in Halifax, in a sponsored symposium. He reviewed the influenza vaccines currently approved in Canada:
- Trivalent inactivated vaccines (TIV): egg-derived and available in standard-dose (SD-TIV), high-dose (HD-TIV), and adjuvanted (aTIV) formulations
- Quadrivalent inactivated vaccines (QIV): egg-derived (SD- or HD-) or cell-derived (SD only)
- Recombinant quadrivalent influenza vaccines (QIVr)
- Live-attenuated trivalent (LAIV3) or quadrivalent (LAIV4) vaccines, administered as a nasal spray
All types have been shown to be safe and effective for preventing influenza infection in most populations; however, only a subset are funded each year through provincial and territorial agencies, based on age group:
- For infants, children, and adults up to age 64 (all provinces and territories): SD-QIV
- Additionally, BC, PEI, and Yukon fund LAIV4 for children aged 2-17; BC funds LAIV4 for adults for whom the injection route of other vaccines is a major barrier
- For adults aged 65 and older:
- BC, Ontario: HD-QIV or TIVa
- Alberta, Saskatchewan, Manitoba, PEI, New Brunswick, Yukon: HD-QIV
- Quebec, Newfoundland and Labrador: SD-QIV
- Nova Scotia, Northwest Territories, Nunavut fund: SD-QIV for the community-dwelling population, HD-QIV for residents of long-term care facilities; Nova Scotia recently announced that HD-QIV access will be extended to the wider senior population next flu season.
“So, it’s actually less confusing at the local level,” concluded Dr. Halperin, “because there’s usually only one vaccine available for each age group. The number of vaccines out there shouldn’t change our message – that people should just get their flu shot."
Insights into Vaccine Efficacy
When assessing vaccine efficacy in subpopulations (e.g., older adults), randomized trials can be costly and have varying results depending on the comparator, the intensity of the specific flu season, and the level of match between the vaccine and the circulating strains. Reviews of evidence across several flu seasons can therefore provide a more comprehensive picture of vaccine efficacy. This approach was taken by Dr. Brenda Coleman, University of Toronto, and her colleagues in their poster about the relative efficacy of aTIV versus HD-TIV in adults aged 65 and up. “[This study was about] wanting to protect the public, especially people over 65 who are at higher risk of the complications that come from being infected with influenza. We wanted to know whether the adjuvanted influenza vaccine was as good as, or better than, other vaccines on the market,” explained Dr. Coleman in an interview. “And it told us that the adjuvanted vaccine was as effective as the high-dose vaccine, with a lower dose of the actual antigen being put into the arm of that recipient.” Across multiple trials covering several pre-COVID-19 flu seasons, there was no significant difference between aTIV and HD- TIV for preventing influenza-related visits to outpatient facilities or hospitals and emergency departments (Figure 2).
Figure 2. Meta-analysis of relative vaccine efficacy for adjuvanted versus high-dose trivalent influenza vaccines in adults aged 65 and older
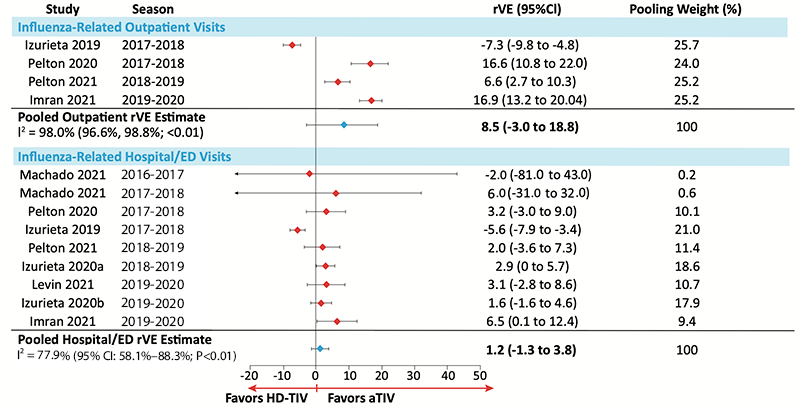
Adapted from Coleman B et al., Poster 74 at CIC 2023
Reflecting on the implications for Canadian clinical practice, Dr. Coleman said, “I think a lot of people don’t know about the differences – I think most seniors do not know that they have a choice, so a lot of them end up getting the regular vaccine that is not adjuvanted and is not high-dose and is not as effective for them. They just might not know enough to ask for it. And I don't know how many healthcare practitioners (HCP) know that either [adjuvanted or high-dose flu vaccine] is more effective than the regular flu shot that younger adults get. Awareness is a major piece of this puzzle.”
Conclusions and Implications for Canadian HCPs and the Public
As the Canadian public and the healthcare system try to return to a more “normal” life following the COVID-19 pandemic, it will be crucial to catch up on any lost momentum toward meeting vaccination targets and improving outcomes. “It's now up to all of us to use and expand upon the tangible legacies of our COVID vaccine experience, along with the equally important processes, collaborations, and relationships that we developed, and apply these into routine vaccination programs throughout the life course,” said Dr. Tam.
When asked for practical advice on how Canadian HCPs and the public can work together to achieve optimal outcomes with influenza vaccination, Dr. Coleman said, “What I want healthcare practitioners to know is that they should be offering either the adjuvanted or the high-dose flu vaccine to their older adults. That's my bottom line. And now that the general public is more knowledgeable about vaccine effectiveness and the fact that there is more than one vaccine out there for a specific disease, they should pay attention to which one they're receiving, and they should be asking for the adjuvanted or the high-dose if they are older.”
Q&A with Dr. Brenda Coleman, Clinical Scientist, Infectious Disease Epidemiology Research Unit, Sinai Health, Toronto
Q: Was there anything in the findings from your meta-analysis that surprised you?
Dr. Coleman: To tell you the truth, I rather expected that high-dose was going to be better [than adjuvanted vaccines]. It's been touted, it's out there, and the governments are buying it more readily than they have been with the adjuvanted vaccine. So I thought it was going to prove to be more effective, but it didn't – [the two types of vaccine] were basically a wash in all of the studies. They’re very similar and we need the healthcare practitioners to know that, and we need our politicians to know that, so there can be a more informed choice.
Q: Is there anything else we still need to know or do, so that we can effectively protect older Canadians from influenza?Dr. Coleman: We just need to get vaccines into arms! They’re not all being vaccinated. They do need to realize how severe influenza can be, and that the vaccines are quite effective at preventing illness and hospitalization.
Q: I know the data in your analysis all come from pre-COVID flu seasons, but I imagine they’re still relevant to our situation now?
Dr. Coleman: Right, now our flu is sort of getting back to normal [compared to 2020-21 when there were few flu infections]. In 2021-22 and in this past flu season, there were a lot more cases of influenza back again, because people weren’t distancing and masking to prevent the spread. One nice thing about the study was that it covered enough different seasons to give us a good breadth to show different circulating strains and different levels of match between the vaccine and the strains.
Q: Are there any lessons from the mass roll-out of COVID-19 vaccines that could be applied to more routine, seasonal immunization programs like influenza?
Dr. Coleman: Trying to vaccinate that many people at once [against COVID-19] was a Herculean task and there were obviously some challenges and delays early on because of limited supply. Now it’s a well-oiled machine that seems to be working just fine. I think now we’re doing the right thing by making vaccines available through pharmacies. It makes vaccination more convenient for a lot of people - whether you walk in and wait for an hour or you make an appointment, you probably won't have to wait as long as you would to see your primary care practitioner. So I think that's a good thing that has happened over the last few years - you can go and get your flu shot and your COVID vaccine with support from your pharmacist, and it makes it a more normal, everyday experience.
This interview has been condensed and edited.